I need to perform the statistical analysis of a health study in the field of nursing, I am in the second year of the master's degree of family nurse practitioner and last year in the subject of resear
Running head: FAMILY KNOWLEDGE ABOUT PALLIATIVE CARE 18
Family Knowledge about Palliative Care
Ernesto Pena Morgado
Ana G. Méndez
NR502: Research Proposal
February Session, 2019
Family Knowledge about Palliative Care
In the United States, the vast majority of palliative care is performed in the home. It is obvious that in this scenario the members of the family play a leading role. Most research related to palliative care in the United States does not describe the level of commitment of the patient and caregivers with such care. (Dillon, 2016).
In a study presented about "How home hospice facilitates patient and family engagement", his author, Dillon, describes how some caregivers cheered for instruction on how to manage their relatives palliative care in relation to the use of the comfort kit, including the management of morphine in relationship to be better prepared to relieve the pain of the patient (Dillon, 2016, pp.595). Another wife described how the education and holistic instruction provided was helpful in dealing with and understanding the care that would be provided to her husband. (Dillon, 2016).
The author concludes that offering instruction and education in relation to such difficult issues as helping to face death, has an important implication in the participation of the patient and the family in palliative care, and is the first necessary step to train patients and the family to make informed decisions (Dillon, 2016).
The hospital-based complex continuous care (CCC) provides care to more than 28,000 Ontarians whose care needs exceed hospital capabilities. It has become necessary to expand these cares to the home environment as well as in long-term care homes (LTC). Therefore, it is a priority that those who provide palliative care are adequately trained to provide experiences of palliative and end-of-life care (EOL) centered on the patient. Training of the family and caregivers should also be done with the aim of facilitating, accelerating and optimizing proper management of these patients in their home environment. (Konietzny & Anderson, 2017).
The studies reviewed agree that the more knowledge you have about these services, the sense of security of people will increase and their cooperation will be more effective, being closely linked positively with their beliefs, knowledge and concerns about palliative care. (Krevers & Milberg, 2015).
However, it has not found any study that demonstrates that the distribution and dissemination of information can modify the perceptions and sense of security regarding palliative care. (Akiyama et al, 2015).
The purpose of the research is to explore the knowledge that have the family members of patients admitted to hospice during the palliative care, and if the implementation of an educational meeting improve the knowledge about the topic.
Significance of the Practice Problem
There are about of 1.6 million Americans benefit annually from palliative care, and the immense majority receive it in the comfort scenario of their home. (National Hospice and Palliative Care Organization [NHPCO], 2015).
The Patients, especially family members, must go through a wide range of complex medical and social situations, however, there is not yet much information on how hospice care could encourage or hinder the commitment to such care. Promoting that patients who can still actively contribute to their care is a valuable achievement that improves health outcomes, the patient's experience and reduces the cost of care (Dillon, 2016). Dillon characterizes the patient's participation in direct care as an "active association" between patients, family members and health professionals (Dillon, 2016, p. 591).
Providing appropriate information about palliative care is vital, as is instilling a sense of security in patients with life-threatening illnesses and their families. Studies have indicated that people’s sense of security is positively associated with their beliefs, knowledge, and concerns about palliative care (Igarashi et al., 2014). However, no empirical studies have investigated whether the distribution of information can alter perceptions and sense of security regarding palliative care. (Krevers & Milberg, 2015).
Research Question
The central question of this investigation would be: “Does the implementation of an educational meeting improve the knowledge of the relatives of terminal ill patients, about the importance and scope of the management and treatment of palliative care”?
P- Family members of patients admitted to palliative care services in St. Sophia nursing care in Miami, over 25 years and under 65.
I- Educational meeting to Family members of patients admitted to palliative care Services.
C- Knowledge of family members about palliative care services, before and after of the educational meeting provided.
O- Increase of the knowledge of family members of patients admitted to palliative care services after the education-instruction given.
The objectives that will assist to answer the research question will be:
1. To identify the knowledge of the relatives of patients with terminal illnesses in relation to the treatment and the scope of their care.
2. To establish if the implementation of an educational meeting improves the knowledge of the relatives of terminal patients in relation to the importance of treatment and the scope of palliative care.
3. Analyze the need to implement periodic educational meetings with family members of patients treated in hospice (continuous care) for terminal illnesses, to improve their knowledge and thereby improve the performance of the nurse who provides the care.
Null Hypothesis: Educational intervention does not improve the knowledge of family members about palliative care
Alternative Hypothesis: Educational intervention is able to improve the knowledge of family members about palliative care.
Theoretical Framework
The most applicable theoretical framework in this study was Lewin's theory, also known as "Lewin's three-step model change management", very applicable to this research because it is the one that most points out the need for change in the knowledge of the family-caregivers on the palliative care of their sick relatives enrolled in this care. Many have criticized this theory for the lack of fluidity and disregard for the dynamic interaction that should exist between the nurse-family and the environment in which care is provided. (Shirey, 2013).
This theory is used by nurses in specialized areas such as palliative care, for various projects to improve quality in the way care is provided to transform care at the bedside. (Wojciechowski, 2016).
1. Defrost or conscientializing the problem, encouraging people (relatives of the sick) to put aside past, inert forms or paradigms that did not lead to any path of success and effective development, breaking the balance or the supposed current stability ( for example: educating them, challenging the St Lewin's theory proposes that people or groups of them (relatives of patients in palliative care) are strongly affected by restraining forces or obstacles (unknowns) that counteract the driving forces (palliative care) aimed at maintaining the status quo of Sick, in turn the driving forces, or positive forces for change, push in the direction that makes the change happen. The tension between these two forces maintains balance. This model consists of the following steps (Wojciechowski, 2016).status quo, showing problems).
2. Change / move, which means going out to find alternatives, demonstrating the benefits of the proposed change and reducing the forces that slow down the change (for example, brainstorming, new models of intervention, training, training).
3. Restart a freeze but now more integrative and stabilize a new equilibrium in the system, making it a habit to resist changes and the negative forces that oppose changes (for example, celebrate success, keep training and monitor changes) and the effectiveness of training and key performance indicators.
Bing shows in the results of your study “Unfreezing the Flexnerian Model: introducing longitudinal integrated clerkships in rural communities” as through the theory of Lewin in the model of change in the three stages mentioned above, achieve with the innovative LIC model, unfreeze the traditional Flexnerian construct for rural areas.
(Bing, 2014, p. 1).
In the same way in this work through the implementation of instruction-education to family members of patients admitted to palliative care, the researcher of this study will demonstrate that knowledge can be increased and the model of change can be trusted in three steps that will help to unfreeze the ignorance of family members regarding palliative care and, in this way, improve the performance of nurses as providers of This care with better results. in the achievement of our objectives.
Synthesis of the Literature
During the review of the bibliography selected to support this study, Kelley & Morrison (2015) in a study published by in the prestigious New England magazine in February 2015, found the main problems that impede accessibility to the palliative care are the multiple perceptions of these services between doctors and patient-caregivers; family-caregivers have the belief that palliative care are exclusive services for the terminals, and that the term palliative care is equivalent to hospice, which would cause patients to react adversely due to the loss of hope. The perceptions of doctors, in a recent survey showed that almost 90% of adults in the United States had no knowledge or had limited knowledge of what palliative care is. (Kelley & Morrison, 2015). Later in that same study, they point out that more than 90% of respondents they would like palliative care for themselves or their families and that they should be universally available. (Kelley & Morrison, 2015).
In another study conducted in India was found that the majority of family-caregivers enrolled in palliative care of their relatives (FCG), 88.6% had a lack of awareness about pain assessment and management, 86.8% of them could not decide how and when to do one intervention, 97.7% had a lack of knowledge about the disease. It was found that in the family-caregivers, 55.1% had a lack of knowledge about the evaluation of pain and its management in cancer. Since FCGs lacked knowledge about the care of cancer patients, there is a need to establish an awareness program to increase knowledge about the evaluation and management of symptoms in patients with cancer. (Nayak et al., 2018).
Reviewing other literatures on palliative care that deals with the need to educate and instruct relatives and patients with cancer about their care, Harden et al. (2017) detected that there is a lack of knowledge and trust among care providers to participate in educational-instructional talks in a meaningful way about palliative care and ignorance among family members and caregivers (p. 233). They concluded that when each facet of the care team and the family understands its role in palliative care, the talks will be early, deep and meaningful and will focus on the patient's objectives, values and preferences and prejudices against palliative care are a potential barrier to quality end-of-life care. (Harden et al., 2017).
The foregoing is argued by studies such as the one carried out in Mumbai, India, where is demonstrated the implications of the education of caregivers in the quality of palliative care. In this study, the need for knowledge in caregivers were evaluated. The results found here show that there are some barriers to the provision and administration of palliative care, among others, the need for more education and training. Participants stated that in many cases they did not feel adequately prepared in the case of relatives to accept one or another form of treatment for them, and expressed the need for additional training in palliative care. (Ghoshal et al., 2018).
There have been few largescale community-wide interventions to distribute appropriate information about palliative care, and no studies have investigated their impact on cancer patients, their families, and the general public. (Akiyama et al., 2015). Akiyama conducted a 3-year community educational intervention and evaluated the effects of distributing such information at the community level, and explored associations among levels of exposure, perceptions, knowledge, and the sense of security achieved. (Akiyama et al., 2015).The results obtained were encouraging in some way and demonstrated the effectiveness of education to improve knowledge about palliative care. Overall perceptions of palliative care, opioids, and receiving care at home improved significantly among the general public and families, but not among the patients at the community level. However, multiple regression revealed that patients of extensive exposure category had significantly more positive perceptions of palliative care to those of no exposure category (Akiyama et al., 2015, p. 348).
Practice Recommendations
In the previous study, the authors Harden et al. (2017), found as a limitation to their work, to know if this project is a sustainable educational method, and on the other hand If nurses continue with educational talks with family members and palliative care patients to improve their knowledge about these services, they will recommend re-evaluating the knowledge of nurses and providers of this care to establish whether the improvement in their knowledge and his educational work was lasting (p 237).
The obstacles to the self-management of patients in palliative care by their family caregivers, found in the study conducted by Schulman-Green et al. (2018), include the lack of understanding both of the different care options (curative / palliative / hospice care), as well as the objectives and goals of the care, that can lead to self-management that does not correspond with the goals of care. In that same study Schulman-Green et al. (2018), a psychoeducational intervention, to caregivers was done with the purpose of improving their knowledge in relation to care options and the objectives of communication of care as part of an auto-management program. In the intervention group, the results showed a mean effect size for a better knowledge of the care options during the first month, with a sustained effect at three months. As regards self-management, the sustained effect was after three months, and a decrease in the burden for the caregiver per month. Those who participated in the intervention talked more frequently with a nurse about the goals of the care and reported less uncertainty and more hope at three months. (Schulman-Green et al., 2018),
The psycho-educational intervention test used: Managing Cancer Care: A Caregiver's Guide (MCC-CG ©) had a preliminary proven efficacy, being well received by the relatives of the patients. As a limitation of the study, they mentioned that the size of the sample was not large enough to be so significant, so they recommended more study among a larger sample to test MCC-CG ©, and simultaneously apply another with a patient intervention: Managing Cancer Care: A Personal Guide (MCC-PT ©), to improve self-management. (Schulman-Green et al., 2018).
In other research conducted and reviewed, the authors refer to the lack of knowledge among patients, care providers and family members. The results demonstrated the insecurity and lack of education among clinical nurses when discussing palliative care with their patients and families, which unquestionably had a negative impact on the performance of nurses when it came to providing hospice care. (Moir et al., 2015). They focused on the educational needs of the nursing staff of hospitalized patients, mentions the difficulty of communicating with family members and patients as an obstacle in the knowledge that they should have to take care of at home. This study showed that less experienced nurses expressed some discomfort when communicating with end-of-life patients and their families, which results in less knowledge of patients and family members about the dilemma they face when they move from palliative care to EoL (End of life). (Moir et al., 2015).
Therefore, the authors recommend that it is necessary to further explore the educational needs among nurses, family members and patients regarding palliative care.
This exploration can lead to the development of educational interventions designed to increase the comfort of nurses by talking to patients and their families and to a greater knowledge of family members and patients in relation to palliative care. As a recommendation, the authors advise for future studies, focus more on assessing the specific educational needs of the enrolled parties in the care, as they are mainly patients and above all family, in this care (Moir et al., 2015).
Project Setting
The project of this work will be carried out in the palliative care staff agency ST. Sophia Nursing Care, in Miami. The mission is to provide Hospice agencies (Compassionate, Kindred, Seasons and Vitas) with the necessary staff to provide highly qualified palliative care, to provide dignified and humane care and help them die with comfort to patients in states terminals of a chronic disease in which they can have up to 6 months of life expectancy, and which can be shortened by an exacerbation or other intercurrent phenomenon. It also has the mission of giving emotional support and helping the families of the sick to deal with the situation, reducing the emotional and economic burden they may assume. There are staff of LPN and RN who provide services in 12 hours of work in 2 shifts; from 8:00 AM to 8:00 PM and 8:00 PM to 8:00 AM for most hospice agencies. In the case of Vitas, which generally, according to the complexity of the cases, place a CNA in the morning shift, the shifts will be from 8:00 AM to 7:00 PM and from 7:00 PM to 8:00 A.M.
In this study I chose Lewin's theory of change as the one that best fits the objectives of the research, because through an educational intervention, it seeks to unfreeze the ignorance that family members have of patients admitted to palliative care, in terms of understanding the management of them, the reason, the objective and the need to apply medicines that promote comfort and help them have a dignified death, without suffering, arguments not very well understood, and that in this way they become a positive factor and collaborator of the multidisciplinary team that supports this care. This structure of change is very well designed and represented by Lewin as already explained in a previous section.
Project Description: methodology
The theoretical framework found most applicable in this study was Lewin's theory also known as "Lewin's three-step model change management” very applicable to this research because it is the one that most points out the need for change in the knowledge of the family of patients enrolled in palliative care.
1. Defrost or conscientializing the problem, encouraging people (relatives of the sick) to put aside past, inert forms or paradigms that did not lead to any path of success and effective development, breaking the balance or the supposed current stability.
This first step coincides in the present study with the phase of unfreezing the old beliefs held by the relatives of patients admitted to palliative care that this care causes an acceleration in the death of their relatives and that the use of drugs at this stage has in the end, this will be done through education and instruction on the objectives of the program.
2. Change / move, which means going out to find alternatives, demonstrating the benefits of the proposed change and reducing the forces that slow down the change (for example, brainstorming, new models of intervention, training, training).
Once the old beliefs of the participants in the study have been defrosted, through the training, training, brainstorming and implementation of educational programs, the benefits obtained by these changes, their relatives and them will be explained; The application of medications to relieve the burden of suffering, the best comfort and the release of relatives from the emotional burden to which they are subjected at this stage.
3. Restart a freeze but now more integrative and stabilize a new equilibrium in the system, making it a habit to resist changes and the negative forces that oppose changes (for example, celebrate success, keep training and monitor changes) and the effectiveness of training and key performance indicators.
In this step 3 we will freeze again but the new ideas already established, with the new behavioral change brought by the new knowledge acquired in relation to palliative care and monitor the persistence of this knowledge to make its stable and lasting learning and replicate it or do it extensive to the rest of the relatives enrolled in this care.
A quantitative observational analytical study will be conducted with a pre-post educational intervention for a maximum of 25 participants, over 25 years and under 65, family of patients with terminal illness who will be admitted to palliative care at St. Sophia hospice agency in Miami, Miami County, in hospice services, to explore the knowledge that participants have about the management and treatment of their family members admitted for palliative care.
The main objective of the study is to know if the educational meeting is able to improve the knowledge of the participants enrolled in the care of their relatives during palliative care. A long-term goal, based on the results, is to implement an educational intervention design to prepare the relatives of patients in palliative care, improving their knowledge about this service.
The participants will be selected by a convenient sample. Criteria for inclusion will be: Spanish-speaking caregivers of patients admitted to palliative care services St. Sophia hospice agency in Miami, Miami County, in hospice services over 25 years and under 65. The exclusion criteria will be those that do not speak Spanish under 25 and over 65 that do not belong to ST. Sophia and not be involved with the palliative care of your sick relative. After the IRB approval, the principal investigator will hold a meeting with authorization from the St. Sophia Home Care agency (Appendix 1- Letter of support) with the aim of explaining to those who will take part in the research, potentially, and who meet the inclusion criteria, that others are willing to participate, the purpose of this study and, at the same time, we will explain to the selected sample, the objectives of this research as well as its benefits, both for their sick relatives and for them. An informed consent will be explained (Appendix-2) to be signed, and an Information to participate in a study / investigation will be presented too (Appendix-3). Informational page A brief survey as a structured instrument of 10 questions pre-test will be taken, with short answers (yes or no), with a maximum of 15 minutes to be completed (Appendix 4) that will assess the knowledge that family members have, enrolled in home care, especially about the management of the sick relative, in this service, its scope and the treatment modalities used. After this a date and time will be agreed upon to hold an educational meeting.
After 15 days there will be another meeting in which they will participate to carry out the education and instruction of 30 minutes, necessary, on the unknown aspects on the subject, they will have 5 minutes to dissipate doubts about the topic, and 15 minutes to apply a post -test in a summative evaluation leading to a final formative evaluation will serve as a way to definitively evaluate whether the implementation of the educational meeting improved the level of knowledge among the participants, and compare the before and after synthesizing the results in numbers. The instrument is valid for the purposes of the objective of the work.
The questionnaire will not include any personal data or private information to prevent breaches of confidentiality. The information will be saved in an office enabled by the principal investigator in duly sealed envelopes. All information will be preserved for a period of no more than 5 years after the study is published. After this time all the documents will be destroyed and discarded. Only the tutor and the principal investigator of the study will have access to the information obtained.
In this study, the variables analyzed will be: Dependent: Knowledge that the relatives of the patients have in relation to the scope of management and treatments during their palliative care. The independent is the educational instructional meeting that will be made to the relatives of the patients. Frequencies and percentages will be used for qualitative variables. A test known as dependent T-test will be applied to the participants to detect significant differences between the recognition scores obtained in the surveys applied to family members, before and after the educational meeting.
According to the IRB criteria, it is essential to maintain the confidentiality and privacy of the participants in an act of respect for human rights. These criteria provide protection through the application of the aforementioned informed consent, before enrolling in the study.
In the same way, the study will be guided by the ethical principles that exist in every investigative process where human beings are enrolled as a vehicle of protection for the participants. The application of these IRB criteria dictates that the protection of human rights is achievable if the study approach complies with the other stipulated criteria of the NHI, FWA, essential to approve the investigation. In addition, the administration of the ST. Sophia agency will be requested the permission to carry out the investigation and ensure that the investigation has been duly approved, and you have all the support and help of the administrative body. All the aforementioned requirements will be obtained before participating in the study in order to protect the human rights of the participants.
The principal investigator will explain that this study has a minimum risk which will be related to fatigue during the completion of the questionnaire. It will be made clear to the participants that if at any time during the investigation they do not feel comfortable with the questionnaire or the education-instruction that will be given and they decide to leave the study, they can do it at any time without implications for their relatives or for they. There will be no benefits or gifts for participating in the recruitment and there will be no monetary rewards before or after the study. But other types of benefits for both the participant, patient, and society would be, obtain knowledge about the care of their relative with terminal illness in palliative care, through the instruction and education received in order to be better prepared to perform and collaborate in the care and management of your relative.
Project Evaluation Results
I will use a package for statistical analysis used in social sciences, known as (SPSS 25) that will be used in order to organize the collected data, validate them and finally analyze them. Frequencies and percentages will be used for qualitative data. I will apply a dependent Student´s T-test distribution because it is a small sample (<30) with population standard deviation unknown, to detect significant differences between the score, before and after the educational meeting about the knowledge of relatives in relation to what concerns palliative care. Indicators of central tendency and dispersion: Medians, Means (M), Standard Deviations (SD) and Standard Errors of the Mean (SEM) will be estimated for quantitative variable.
Taking into account the objective for which this study was designed, we hope that with the educational meeting could improve the knowledge of the relatives of admitted patients for palliative care, attending to the areas where this knowledge will be more deficient. Notwithstanding this achievement, we know in advance that we will have to face some limitations that the research has, such as the small sample selected, as well as the method of selection of the sample that was convenient, which we know is not a scientific sample. A sampling bias will be expected. In the same way, having worked with the Spanish speaking population to be the majority in the city of Miami, limits the cultural and religious characteristics and beliefs of the sample, which can be a variable that could be of great influence on the results with a potential of bias not studied because it is not an interest of the author for this work, which limits the conclusions to which we can finally arrive, and the generalization of the results in the surveys.
The evaluation process will involve both the formative and summative evaluation approaches. Formative evaluation will take place during the implementation process. It will, therefore, occur during the preliminary project stages. Likewise, the formative assessment will also take place during the progress of the project. Besides, this formative evaluation will involve the assessment of whether the implementation of educational meetings improve the level of knowledge amongst family members of patients admitted to palliative care. The outcomes realized from such a preliminary formative evaluation before the intervention sets the baseline findings for the whole study. The influence of the educational meetings implementation is assessed depending on the current PICO question that was mentioned above. On the other side, a summative evaluation takes place after the intervention process. The evaluation of these PICO questions occurs following the implementation of the educational meetings whereby questionnaires will be re-administered to family members of patients admitted to palliative care over 25 years old and under 65.
Results obtained before and after the educational meeting is analyzed and will undergo a summative evaluation to come up with conclusive findings. Therefore, outcomes realized from the study will be evaluated in line with the PICO questions. Such evaluation enables to examinates of whether the project has achieved the expected research findings or not. Relevantly, the summative evaluation will besides entailing in an evaluation of whether it would be beneficial to establish a long-term objective which will involve the establishment of educational meeting for all new admitted patients for palliative care.
Notwithstanding the above, we can anticipate that an educational meeting will be able to improve the knowledge of the relatives of patients receiving palliative care and who are actively enrolled in their management as part of the team. This will help them to better understand the objective of these cares, their general management and the justification of the treatment in the way of supporting the symptoms that generated the care, and with them we can give a more efficient support to the needs of these patients in its final stage, effectively administering dignified and human care, the central objective of care in these stages. With this achievement we can replicate this study and magnify it in order to universalize the knowledge in this field that increasingly increases its usefulness and use, especially in the home setting, with the economic savings for the family, and institutions, and decrease in the emotional burden for family caregivers.
Discussion and Implications for Nursing and Healthcare
Studies that demonstrate the implications of the education of practitioners and caregivers in the quality of palliative care, is argued in a study that was conducted in Mumbai, India, where the need for knowledge in the caregivers was evaluated. The results found here show that there are some barriers to the provision and administration of palliative care, among others; the need for more education and training. Participants stated that in many cases they did not feel adequately prepared to carry out discussions and interventions on patients or in the case of relatives to accept one or another form of treatment for them, and expressed the need for additional training in palliative care. (Ghoshal et al., 2018).
In a review conducted of an investigation carried out in the United Kingdom, it was determined that education and training through instruction were identified as important facilitators of collaborative work within the components of the palliative care team, fundamentally among caregivers. There are many studies that identify education for generalists and caregivers as a priority. (Hudson, P., Quinn, K., Ohanlon, B., & Aranda, S. 2008).
There is a clear need to develop and implement educational interventions to support palliative care providers and their families in the management and treatment of these patients and how to address the additional significant barriers of the unique "cure-oriented" culture of mentalities of the doctors, ensuring that this also has a positive impact in remodeling the mentality of the relatives in relation to what is handled as palliative care, so that this way it also positively impacts the practice of nursing that in the end are the executors of these careful . All the advantages explained, of achieving greater instruction, will result in optimizing the care and performance of nursing in palliative care.
We recommend continuing to expand studies aimed at exploring the knowledge in family members of patients admitted to palliative care with larger samples, representative of more diverse populations and to add behavioral studies of variables that may hinder the acquisition of knowledge, using modalities of sample selection scientific studies, which are representative of the populations studied
Plans for Dissemination
From the most recent practical evidence in the field of research has shown that when disseminating the information and results of a research study is more effective to use different types of media. In this study, face-to-face interaction will be an important resource to fulfill the purpose of generalizing the results of the study. For this purpose, a Power Point presentation of no more than 30 minutes will be presented in which a practical summary of the whole study will be presented to classmates and the teacher. A copy will also be delivered in Word and another with Poster design. The poster will include a summary information in consideration of the complete study. A copy of the complete study will be delivered to the library of Ana G. Mendez University, South Florida Field for anyone who wants to learn about the information provided.
Summary and Conclusion
As stated in the introduction, the purpose of the research is to explore the knowledge that have the family members over 25 years old and under 65 of patients admitted to hospice during the palliative care, and if the implementation of an educational meeting improve the knowledge about the topic.
So far it has been possible to understand in the bibliography reviewed ignorance that exists among the caregivers who are enrolled in the palliative care of their relatives, as a main part of the team that provides this care, usually in the home setting. This lack of knowledge has been verified in our professional performance and was what generated our concern that led to this study. However, there is a need to complete other studies aimed at obtaining more information about other variables such as cultural level and cultural or religious beliefs that could affect the acquisition of knowledge about this care, in the family. The instrument designed to explore this knowledge will allow us to guide, build and implement an educational-instructional meeting aimed at improving the areas of ignorance, and at the same time determine if it was valid and effective to be disseminated and finally implemented. In this way it is expected to be able to improve care services and thereby achieve the objectives of this care; more comfort for the patient and decrease the economic and emotional burden of the caregivers
.
References
Akiyama, M., Hirai, K., Takebayashi, T., Morita, T., Miyashita, M., Takeuchi, A., Eguchi, K. (2015). The effects of community-wide dissemination of information on perceptions of palliative care, knowledge about opioids, and sense of security among cancer patients, their families, and the general public. Supportive Care in Cancer, 24(1), 347-356. doi:10.1007/s00520-015-2788-4
Bing-You, R. G., Trowbridge, T. L., Kruithoff, C., & Daggett Jr, J. L. (2014). ORIGINAL RESEARCH. Unfreezing the Flexnerian Model: introducing longitudinal integrated clerkships in rural communities. Rural & Remote Health, 14(3), 1–12. Retrieved from https://librarylogin-um.suagm.edu/login?url=https://search-ebscohost-com.librarylogin-um.suagm.edu/login.aspx?direct=true&db=ccm&AN=103896599&site=ehost-live
Dillon, E. C. (2016). How home hospice care facilitates patient and family engagement. Death Studies, 40(10), 591-600. doi:10.1080/07481187.2016.1203377.
Ghoshal, A., Damani, A., Dighe, M., Dhiliwal, S., & Muckaden, M. (2018). Exploring education and training needs in palliative care among family physicians in Mumbai: A qualitative study. Indian Journal of Palliative Care, 24(2), 139. doi:10.4103/ijpc.ijpc_216_17
Harden, K., Price, D., Duffy, E., Galunas, L., & Rodgers, C. (2017). Palliative Care: Improving Nursing Knowledge, Attitudes, and Behaviors . Clinical Journal of Oncology Nursing, 21(5). doi:10.1188/17.cjon.e232-e238.
Hudson, P., Quinn, K., Ohanlon, B., & Aranda, S. (2008). Family meetings in palliative care: Multidisciplinary clinical practice guidelines. BMC Palliative Care, 7(1). doi:10.1186/1472-684x-7-12.
Igarashi A et al (2014) A population-based survey on perceptions of opioid treatment and palliativecare units:OPTIM study. AmJ Hosp Palliat Care 31(2):155–160
Kelley, A. S., & Morrison, R. S. (2015). Palliative Care for the Seriously Ill. New England Journal of Medicine, 373(8), 747-755. doi:10.1056/nejmra1404684.
Konietzny, C., & Anderson, B. (2017). Comfort Conversations in Complex Continuing Care: Assessing Patients’ and Families’ Palliative Care Needs. Perspectives: The Journal of the Gerontological Nursing Association, 39(4), 14–22. Retrieved from https://librarylogin-um.suagm.edu/login?url=https://search-ebscohost-com.librarylogin-um.suagm.edu/login.aspx?direct=true&db=ccm&AN=129270264&site=ehost-live.
Krevers, B., & Milberg, A. (2015). The Sense of Security in Care—Relatives Evaluation Instrument: Its Development and Presentation. Journal of Pain and Symptom Management, 49(3), 586-594. doi:10.1016/j.jpainsymman.2014.06.019
Moir, C., Roberts, R., Martz, K., Perry, J., & Tivis, L. (2015). Communicating with patients and their families about palliative and end-of-life care: Comfort and educational needs of nurses. International Journal of Palliative Nursing, 21(3), 109-112. doi:10.12968/ijpn.2015.21.3.109.
National Hospice and Palliative Care Organization [NHPCO]. (2015). NHPCO’s facts and figures: Hospice care in America. Retrieved from http://www.nhpco.org/sites/ default/files/public/Statistics Research/2013_Facts_Figures. pdf
Nayak, M., George, A., & Vidyasagar, M. (2018). Perceived barriers to symptoms management among family caregivers of cancer patients. Indian Journal of Palliative Care, 24(2), 202. doi:10.4103/ijpc.ijpc_27_18.
Schulman-Green, D., Linsky, S., Jeon, S., Kapo, J., Ercolano, E., Jeuland, J., & Mccorkle, R. (2018). Improving Cancer Family Caregivers Knowledge of Care Options and Goals of Care Communication: Results From a Pilot RCT. Journal of Pain and Symptom Management, 56(6). doi:10.1016/j.jpainsymman.2018.10.317.
Shirey, M. R. (2014). Lewin's theory of planned change as a strategic resource. Journal of Nursing Administration, 43(2), 69-72. doi: 10.1097/NNA.0b013e31827f20a9
Wojciechowski, E., Murphy, P., Pearsall, T., French, E. (2016). A Case Review: Integrating Lewin's Theory with Lean's System Approach for Change. Online Journal of Issues in Nursing, 10913734, Vol. 21, Issue 2.
Appendix -1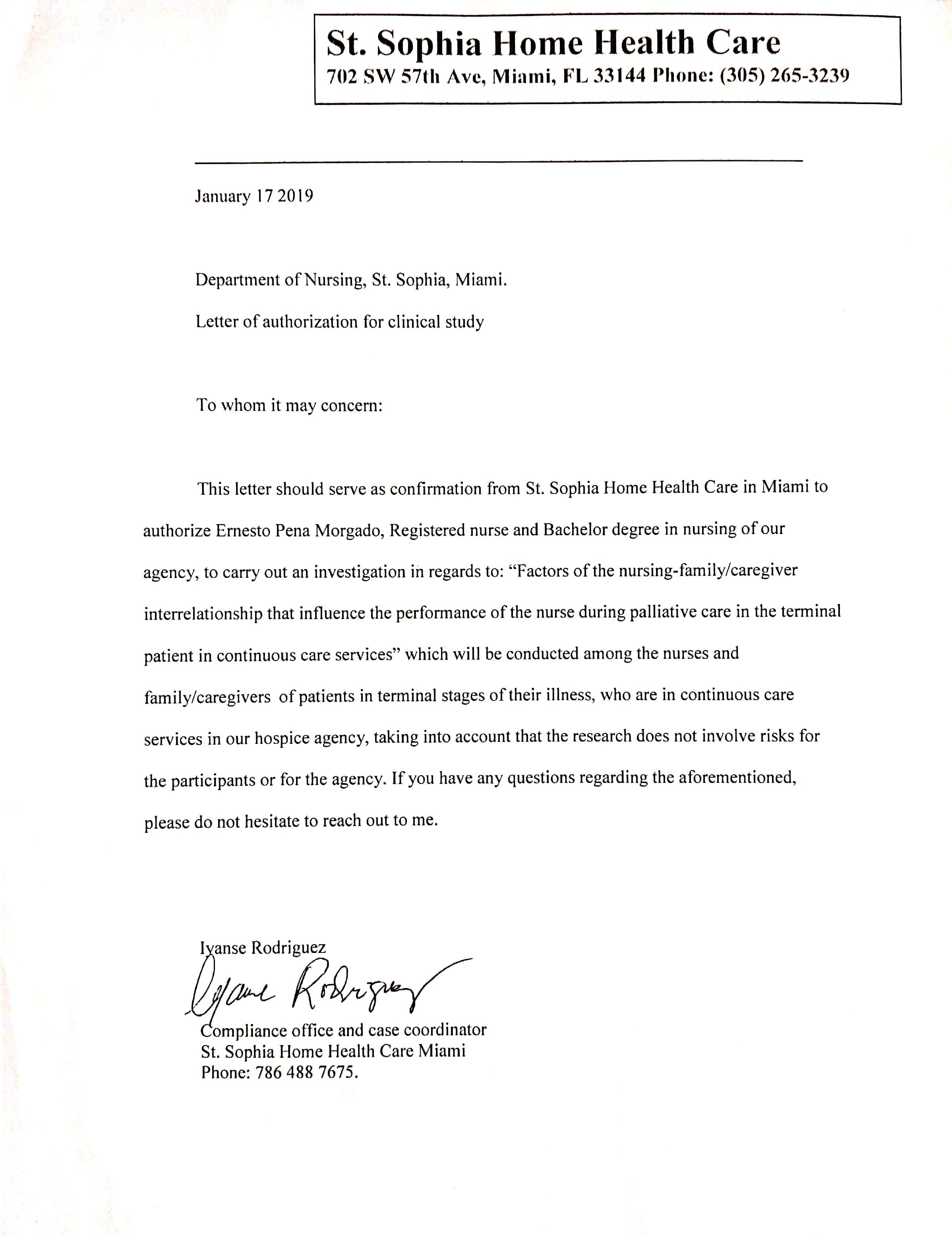
Appendix- 2
UNIVERSIDAD ANA G. MENDEZ
South Florida campus
MSN Program
Consentimiento informado para un estudio con riesgo mínimo
Family knowledge about palliative care
Descripción del estudio y el rol de su participación
Ernesto Pena lo está invitando a participar en un estudio de investigación. Ernesto Pena, Investigador Principal y Profesora Nancy Woelki, de la Universidad Ana G. Méndez (UAGM) [SFC]. El propósito de esta investigación es conocer el conocimiento que tienen los familiares de los pacientes con enfermedades terminales, atendido en cuidados paliativos.
Su participación en esta investigación consistirá en dedicar 10 minutos para leer y discutir este consentimiento informado a los participantes que fueron escogidos para participar y que cumplan con los criterios para participar en este estudio. Posterior a ello se tomará una breve encuesta de no más de 10 preguntas con respuestas cortas (sí o no) para explorar el conocimiento que tienen los familiares de los pacientes con enfermedades terminales, admitidos en hospicio, para proveerles cuidados paliativos. Después de 15 días se dará otra reunión en la que participarán para realizar la educación e instrucción de 30 minutos, necesaria, sobre los aspectos desconocidos sobre el tema, tendrán 5 minutos posteriores para disipar dudas sobre el tópico, y 15 minutos para aplicar un post-test para conocer la efectividad de la educación que se les dará ese mismo día.
A usted le tomará aproximadamente una hora y quince minutos para completar este estudio.
Riesgos e Incomodidades
Hasta el momento el posible riesgo es el agotamiento que puede haber durante el proceso de responder las preguntas y analizar los examen y escuchar la conferencia. Sin embargo no debe preocuparse, pues si en algún momento de la investigación, usted no se siente confortable con las preguntas y decide no continuar siendo parte del estudio, usted puede abandonar el proyecto en cualquier momento.
Posibles Beneficios
El principal beneficio que se obtendrá con su participación en esta investigación es poder conocer los principales aspectos relacionados con el cuidado de pacientes con enfermedades terminales en cuidados paliativos, en los que los familiares enrolado en estos cuidados, tienen mayor desconocimiento, y poder dar instrucción y educación sobre ellos, para de esta forma el familiar esté de acuerdo en la manera en que se realicen los cuidados y el manejo terapéutico, comprenda el objetivo y la razón para estos cuidados y todo lo concerniente al manejo de los pacientes y de qué forma los familiares pueden cooperar e insertarse de forma efectiva en los cuidados del enfermo. La información obtenida en el cuestionario no incluye los nombres de los participantes y se conservarán por un período de 5 años; se guardarán bajo llave en la oficina del hogar del Investigador Principal en sobres separados. Después de cinco años, todo cuestionario será destruido por una trituradora de papel y serán descartados.Tendrán acceso a los cuestionarios el Investigador Principal y su mentora. También se protegerá la confidencialidad de los participantes enfatizando en todo momento sobre la importancia de mantener toda información anónima. No se requerirá que los participantes incluyan sus nombres en los cuestionarios ni los participantes serán identificados en ningún informe sobre el estudio”.
Protección de la Privacidad y Confidencialidad
Toda información relacionada a su identidad será manejada de manera privada y confidencial y será protegida en todo momento. Bajo ninguna circunstancia se compartirá información del participante con terceros. Los datos recopilados se guardarán en un lugar privado, seguro y bajo llave. Cualquier documento recopilado será almacenado en la casa del investigador principal por un periodo de cinco (5) años. Los mismos estarán bajo la tutela del investigador principal Ernesto Pena. Después de un periodo de 5 años, la información será destruida (triturada).
Decisión sobre su participación en este estudio
Su participación en este estudio es totalmente voluntaria. Usted tiene todo el derecho de decidir participar o no de este estudio. Si usted decide participar en este estudio tiene el derecho de retirarse en cualquier momento sin penalidad alguna.
Información contacto
Si usted tiene alguna duda o inquietud correspondiente a este estudio de investigación o si surge alguna situación durante el periodo de estudio, por favor contacte a Ernesto Pena, [email protected] al (786) 291-0564. Si usted tiene preguntas sobre sus derechos como sujeto de investigación por favor comuníquese con la Oficina de Cumplimiento de la Investigación del UAGM al 787-751-3120 o [email protected].
Consentimiento
He leído este documento y se me ha dado la oportunidad de aclarar todas las dudas relacionados con el mismo. Por esta razón estoy de acuerdo en participar en esta investigación.
______________________ ________________________ ________________
Nombre del Participante Firma mes/día/año
________________________ __________________________ ________________
Nombre del Investigador Principal Firma mes/día/año
NOTA:
Es nuestra responsabilidad proveerle con una copia de este documento. Favor de seleccionar la opción de su preferencia.
Certifico que se me entregó copia de este documento.
Certifico que se me ofreció copia de este documento y no deseo tener copia del mismo.
Appendix- 3 Information to participate in a study / investigation. Informational page
UNIVERSIDAD ANA G. MENDEZ
South Florida campus
MSN Program
Información para participar en un estudio/investigación
Hoja Informativa
Family knowledge about palliative care
Descripción del estudio/investigación y tu participación en el mismo
Se realizará un estudio cuantitativo observacional analítico con una intervención educativa y un test pre-post, a un máximo de 25 familiares de pacientes con enfermedad terminal que serán admitidos en cuidados paliativos en la agencia de cuidados paliativos St. Sophia en Miami, Condado de Miami , para explorar el conocimiento que los participantes tienen sobre el manejo de sus familiares- pacientes en este servicio, así como en el uso de medicamentos para controlar los diferentes síntomas de ellos. La encuesta será aplicada por el investigador Principal exclusivamente el cual se encargará únicamente de procesar los datos de los test pre y post a la reunión educativa que será impartida únicamente por el investigador principal.
El objetivo principal del estudio es saber si la reunión educativa puede mejorar el conocimiento de los participantes enrolados en el cuidado de sus familiares, durante los cuidados paliativos. Un objetivo a largo plazo, basado en los resultados, es implementar un diseño de intervención educativa para preparar a los familiares de los pacientes en cuidados paliativos, mejorando su conocimiento sobre este servicio.
[Este no es un documento llena blanco, por lo que es importante leer e incluir la información que se le solicita].
Ernesto Pena estudiante y la Profesora Nancy Woelki, mentor, le invita a formar parte de un estudio de investigación cuantitativo analítico observacional que tendrá como objetivo conocer que conocimiento tienen los familiares de pacientes admitidos en servicios de cuidados paliativos para implementar una reunión educativa-instructiva con el propósito de mejorar el conocimiento que esté deficiente en relación a el manejo general de los sus familiares enfermos durante estos cuidados, asi como el fundamento de los tratamientos para el control de los síntomas y poder examinar la efectividad de la educación impartida. El propósito de este [estudio/investigación] es [“explique en un lenguaje sencillo que pueda ser entendido fácilmente”].
Su participación en este [estudio/investigación] consistirá en dedicar 10 minutos para leer y discutir este consentimiento informado a los participantes que fueron escogidos para participar y que cumplan con los criterios para participar en este estudio. Posterior a ello se tomará una breve encuesta de no más de 10 preguntas con respuestas cortas (sí o no) para explorar el conocimiento que tienen los familiares de los pacientes con enfermedades terminales, admitidos en hospicio, para proveerle servicios de continuos careo cuidados paliativos. Después de 15 días se dará otra reunión en la que participarán para realizar la educación e instrucción de 30 minutos, necesaria, sobre los aspectos desconocidos sobre el tema, tendrán 5 minutos posteriores para disipar dudas sobre el tópico, y 15 minutos para aplicar un post-test para conocer la efectividad de la educación que se les dará ese mismo día. [Describa los procedimientos en un lenguaje sencillo que pueda ser entendido fácilmente”].
Le tomará aproximadamente una hora y quince minutos para completar este estudio. [indique un tiempo estimado] participar de este [estudio/investigación].
Riesgos e Incomodidad
Hasta el momento el posible riesgo es el agotamiento que puede haber durante el proceso de responder las preguntas y analizar los examen y escuchar la conferencia. Sin embargo no debe preocuparse, pues si en algún momento de la investigación, usted no se siente confortable con las preguntas y decide no continuar siendo parte del estudio, usted puede abandonar el proyecto en cualquier momento.
[No conocemos de ningún riesgo e incomodidad que le pueda ocasionar el participar en este[estudio/investigación] –O-[Existe algún riesgo e incomodidad que pueda resultar de participar en este [estudio/investigación]. Estos pueden ser [describa cualquier riesgo o incomodidad que pueda ocurrir de participar en este estudio] [Indicar que medidas se tomarán para minimizar estos riesgos e incomodidades]
Posibles Beneficios
El principal beneficio que se obtendrá con su participación en esta investigación es poder conocer el manejo y la justificación para el tratamiento de los síntomas fundamentales de su familiar enrolado en los cuidados paliativos, para de esta forma que aumente su conocimientos sobre los cuidados que se le proporcionan a su familiar y de qué forma los familiares pueden cooperar e insertarse de forma efectiva en los cuidados del enfermo [Describa el beneficio que obtendrá el participante o cualquier otra persona al participar de este estudio] -O- [“No tenemos conocimiento que al participar de este estudio usted
Tenga algún beneficio”. [De ser apropiado, puede añadir: “Este estudio/investigación le puede ayudar a entender…” (Debe ser breve)].
Incentivos
(El investigador debe describir cualquier incentivo que vaya ofrecer para promover la participación en el estudio). (ej., dinero, regalos, cursos o créditos). [Si no ofrecerá incentivos puede omitir esta sección.]
(Si el investigador está ofreciendo créditos por su participación en esta investigación, debe especificar que esos créditos también están disponibles realizando otro tipo de actividades que no sean de investigación y que emplean la misma cantidad de esfuerzo y de tiempo. El investigador puede referir al participante a otras personas para recibir información al respecto. [Si no ofrecerá créditos por la participación puede omitir esta sección.]
Protección de la Privacidad y Confidencialidad
Toda información relacionada a su identidad será manejada de manera privada y confidencial y será protegida en todo momento. Bajo ninguna circunstancia se compartirá información del participante con terceros. Los datos recopilados se guardarán en un lugar privado, seguro y bajo llave. Cualquier documento recopilado será almacenado en la oficina de la casa del investigador principal por un periodo de cinco (5) años en sobres separados. Los mismos estarán bajo la tutela del investigador principal Ernesto Pena. La información obtenida en el cuestionario no incluye los nombres de los participantes. Después de cinco años, todo cuestionario será destruido por una trituradora de papel y serán descartados. Tendrán acceso a los cuestionarios el Investigador Principal y su mentora. También se protegerá la confidencialidad de los participantes enfatizando en todo momento sobre la importancia de mantener toda información anónima. No se requerirá que los participantes incluyan sus nombres en los cuestionarios ni los participantes serán identificados en ningún informe sobre el estudio”.
(Describa el grado de confidencialidad que se le dará a los datos de los participantes que deseen ser parte del estudio).
Decisión sobre su participación en este estudio
Su participación en este estudio es totalmente voluntaria. Usted tiene todo el derecho de decidir participar o no de este estudio. Si usted decide participar en este estudio tiene el derecho de retirarse en cualquier momento sin penalidad alguna.
Información contacto
Si usted tiene alguna duda o inquietud correspondiente a este estudio de investigación o si surge alguna situación durante el periodo de estudio, por favor contacte a Ernesto Pena, [email protected], o al teléfono (786) 291-0564. Si usted tiene preguntas sobre sus derechos como sujeto de investigación por favor comuníquese con la Oficina de Cumplimiento en la Investigación del SUAGM al 787-751-3120 o [email protected].
Una copia de esta carta informativa le será entregada.
Appendix- 4
Cuestionario (Questionnaire)
| Preguntas | Sí | NO |
| 1- Conoce que son los cuidados paliativos? | ||
| 2- Conoce que significa tener una enfermedad crónica en estado avanzado o terminal? | ||
| 3. Conoce porque su familiar ha sido puesto en cuidados paliativos? | ||
| 4. Conoce usted que objetivo tiene los cuidados paliativos? | ||
| 5. Conoce usted los síntomas principales que van a ser controlados? | ||
| 6- Conoce los tratamientos que recibirá su familiar y como trabajan esos medicamentos. | ||
| 7. Está de acuerdo con que su familiar reciba morfina u otros opioides y/o sedantes e hipnóticos? | ||
| 8. Alguien le explicó cuál es el alcance de los cuidados, hasta donde se puede llegar y hasta donde no? | ||
| 9. Conoce sus derechos y deberes en los cuidados como familiar? | ||
| 10. Conoce como se manejan los cuidados paliativos en su familiar específicamente? |



