Final Assignment For the Final Assignement, you will prepare a four- to five-minute audiovisual presentation on a health informatics topic that includes the following: Audiovisual format: To meet th
Chapter 31 Future Directions and Future Research in Health Informatics
Nancy Staggers
Ramona Nelson
David E. Jones
Health informatics can be described as an interprofessional discipline that is grounded in the present while planning for the future.
Objectives
At the completion of this chapter the reader will be prepared to:
1.Explore major trends and their implications for future developments in healthcare, health informatics, and informatics research
2.Analyze techniques and challenges of planning for future directions and trends
3.Apply futurology methodologies in identifying trends and possible, probable, and preferred futures
4.Describe the field of nanotechnology and its subdisciplines, the role of informatics in nanotechnology, and implications for healthcare
5.Analyze the advantages and disadvantages of nanotechnology in health and health informatics
Key Terms
Backcasting, 499
Cytotoxicity, 505
Data visualization, 502
Extrapolation, 497
Futures research, 495
Nanofabrication, 503
Nanoinformatics, 505
Nanomedicine, 504
Nanotechnology, 502
Trend analysis, 497
Abstract
This chapter expands on the future directions sections included in the individual chapters to provide broad guidance about the future of informatics. First, healthcare trends in society are outlined. Second, futures studies or futurology (methods to analyze probable future directions in any field) is discussed. Third, an overview of potential future directions in informatics are discussed, including the following informatics trends: (1) patient engagement, consumerism, and informatics; (2) electronic health records (EHRs) 2.0; (3) usability and improving the user health information technology (health IT) experience; (4) big data and data visualization; and (5) nanotechnology and nanoinformatics. The last trend is discussed in more detail as an example of the major influence each of these trends will likely have on the future of healthcare and society as a whole. The organization and depth of the nanotechnology-related content also provides a guide for readers to develop similar material in informatics areas of specific interest.
Introduction
Informatics will play a large role in the future of healthcare. Which informatics trends will prevail and in what depth is unclear. In each of the chapters in this book authors outlined expanding areas of influence, from knowledge discovery to the epatient, from cloud computing to standards integration with public health data sharing, and from initial EHR installations to mobile health. In this chapter unequivocal healthcare trends are listed, followed by methods that readers may use to predict likely trends in the future. These techniques are called futurology or futures research methods. Subsequently, five major trends are discussed: (1) patient engagement, consumerism, and informatics; (2) EHRs 2.0; (3) usability and improving the user experience for health IT; (4) big data and data visualization; and (5) nanotechnology and nanoinformatics. Special attention is given to nanotechnology and nanoinformatics.
The purpose of informatics is to provide support for clinical care, public health, and other practices. Thus to understand the future of health informatics, major health trends need to be acknowledged. Examples of unequivocal trends in society include:
•Rising healthcare costs. In the U.S. alone, costs are expected to nearly double to $4.5 trillion by 2019, up from $2.5 trillion in 2009.1
•Aging populations. By 2050 the global population of those aged 60 years or older will be more than 2 billion.2
•Increase in patients with chronic diseases. By 2030 chronic diseases will be the leading cause of deaths worldwide.3 Diabetes rates alone will increase by 2.8% to 4.4%.4
•Predicted shortage of healthcare providers. By 2025 the U.S. will have a shortage of an estimated 260,000 registered nurses5 and 124,000 physicians.6
•Health insurance reform. Several health reform measures are scheduled to take effect in 2014, according to the provisions of the Patient Protection and Affordable Care Act signed into law on March 10, 2010.7
These trends clearly have implications for informatics support in the future but how does one determine or perhaps even create future trends? Futures research or futurology, the methods used to determine future trends in any field, may help to answer this question.
Futures Research or Futurology
Health informatics can be described as an interprofessional discipline that is grounded in the present while planning for the future. Health informatics specialists are selecting and implementing today's healthcare information systems, thereby creating the foundation for the systems of tomorrow. By reviewing current trends and predictions, as well as employing tools for predicting and managing the future, health informatics specialists can prepare for their leadership role in planning for the effective and innovative healthcare information systems of the future. This section introduces the reader to levels of change that can be anticipated in future trends. By analyzing methodologies and tools for predicting, planning for, and managing the future, health informatics specialists are introduced to the kind of leadership roles they will play in planning future healthcare information systems. With a better understanding of the potential future, informatics professionals can make better current decisions.
Defining Futures Research or Futurology
Futures research is the rational and systematic study of the future with the goal of identifying possible, probable, and preferable futures. The formal study of the future goes by a number of names, including foresight and futures studies, strategic foresight, prospective studies, prognostic studies, and futurology. Using a research approach to formally study the future began after World War II. Since that time a number of institutes, foundations, and professional associations were established supporting the field of futures studies. Examples of these are included in Box 31-1. However, from the beginning, this field of study aroused skepticism. Today researchers and corporate strategists may use numerous concepts, theories, principles, and methods that are based on the field of futures research but they may not associate these methods with the field of futurology.8 A number of educational programs related to futures studies now use the various futurology terms to describe their programs. Box 31-2 includes examples of educational programs related to this field. Despite the initial skepticism about the topic, today the futures studies techniques are accepted, educational programs are available, and these methods can be very useful for informaticists.
The focus of futures studies has evolved over time. Initially, futures studies tended to focus on a longer time horizon of at least 10 years. Today researchers are typically studying the world anywhere from 5 to 50 years from now.9 This creates an overlap of futures studies with traditional forecasting and planning disciplines that examine political, economic, and market trends on a 1- to 5-year horizon.
Health informatics can use traditional forecasting and planning methods in combination with futures studies methods as well as futures studies. Strategic planning in health informatics typically focuses on projects 1 to 3 years in the future. Institutional long-range planning tends to focus on 5 to 10 years in the future. For example, vendor contracts for major healthcare informatics systems often cover a 5- to 10-year period spanning both strategic and long-range planning. However, there are some differences between forecasting and futures studies.
First, forecasters focus on incremental changes from existing trends while futurists focus on systemic, transformational change. Second, futurists do not offer a single prediction. Rather, they describe alternative, possible, and preferable futures, keeping in mind that the future will be created, in most part, by decisions made today. The technical, political, and sociocultural infrastructure being built today will have a major impact on the choices of tomorrow. Both types of change are key to planning health informatics products.10 Understanding the impact of future trends and using this information for planning begins by understanding the degree and scope of change that occurs over time.
Box 31-1 Futures Studies: Selected Associations, Institutes, and Foundations
• Acceleration Studies Foundation, http://accelerating.org/index.html
• Copenhagen Institute for Future Studies, www.cifs.dk/en/
• Foresight Canada, www.foresightcanada.ca/
• Fullerton and Cypress Colleges, and School of Continuing Education: Center for the Future, http://fcfutures.fullcoll.edu
• The Arlington Institute, www.arlingtoninstitute.org
• Association of Professional Futurists, www.profuturists.org
• The Club of Rome, www.clubofrome.org
• The Futurist, www.wfs.org/futurist/about-futurist
• Institute for the Future, www.iftf.org/home
• The Millennium Project, www.millennium-project.org
• World Future Society, www.wfs.org/node/920
• World Futures Studies Federation (WFSF), www.wfsf.org
Box 31-2 Selected University Programs in Futures Studies
• EBS Business School: Institute for Futures Studies and Knowledge Management, www.ebs.edu/11866.html?&L=1
• Regent University: School of Business & Leadership, www.regent.edu/acad/global/degree_programs/masters/strategic_foresight/home.cfm
• TamKang University: Graduate Institute of Futures Studies, http://future.tku.edu.tw/en/1-4.htm
• University of Advanced Technology, http://majors.uat.edu/Emerging-Tech
• University of Hawaii: Hawaii Research Center for Futures Studies, www.futures.hawaii.edu/academic-offerings.html
• University of Houston: College of Technology, www.houstonfutures.org/program.html
• University of Stellenbosch: Institute for Futures Research, www.ifr.sun.ac.za/Home
• University of Turku: Finland Futures Research Centre (FFRC), www.utu.fi/en/units/ffrc/Pages/home.aspx/
Future Directions and Level of Change
The 1890 United States census count was finished months ahead of schedule and far under budget by using a punch card counting machine. This technology continued to be used by the U.S. Census Bureau well into the 1950s because the problem to be solved remained basically unchanged. Each decade, the Census Bureau was challenged to count the number of people in the population and certain characteristics about the population. Over the decades the population characteristics to be counted changed but the need to count these data remained the same.
In the 1950s the Census Bureau introduced new technology in the form of computers and magnetic computer tape. The basic problem remained the same but new technology offered more efficient and effective methods for solving that problem. The Census Bureau's introduction of new technology is an example of a first-level change. With a first-level change a new technology solves a problem in a more efficient or effective manner.
For example, replacing a typewriter with a word processer is an example of a first-level change. One is still producing a document but the technology makes the process more effective and efficient. Another example is the use of Bar Code Medication Administration (BCMA) methods. Scanning a bar code before administering medication can make the process of administering medication safer. However, scanning bar codes does not change the basic role or responsibility of healthcare providers. Within the levels of change, first level change is the least disruptive and the most comfortable level of change. In many ways requests that new technology be designed to fit the work-flow of healthcare providers is, in reality, a request, or perhaps a demand, for first-level change only. In fact, if the equipment and related procedures do not support the current roles and responsibilities of the healthcare providers, they quickly develop workarounds to meet their requirements that the degree of change be limited to a first-level change.
A second-level change involves changing how a specific outcome is achieved. For example, historically the peer review process used by professional journals involved sending a submitted manuscript to a limited number of selected experts for an anonymous opinion. The goal was to ensure that only the highest quality articles were published. The process of review and revision could take several weeks or months. In addition, with a limited number of experts screening what is published, some degree of professional censorship existed. Articles representing a paradigm shift in thinking risked being rejected as not on target by a limited set of reviewers. Today, professional online journals, where all readers can comment on material, are changing who is involved and how the peer review process is completed, with comments from readers assuming a more important role than in the past. Similarly, patient groups within social media applications are changing how patients learn about their health problems. Groups of patients help each other to read and interpret the latest research to create a whole new level of health literacy within these groups. Social media interactions not only change the process for achieving an outcome, but also change the relationships between the participants. For example, as patients become organized and knowledgeable, they take a more active role in their own care and move from the role of patients needing education about their diseases into more of a colleague role, sharing new and innovative findings with healthcare providers.
The scope of change at this level creates both excitement and anxiety within professional groups and among individual healthcare providers. The scope of practice, policies, procedures, and established professional customs, such as professional boundaries, are challenged and resistance to this challenge can be expected. For example, in healthcare the goals of improved health for individuals, families, groups, and communities have not changed but technology is changing the roles and responsibilities related to how these goals might be achieved.
A third-level change alters the process and can also refocus the goal. For example, a hyperlinked multimedia journal, with a process for adding reader comments and linking to related publications, may change not only the definition of an expert, but also the historical gold standard for review of new information and knowledge. Another example can be seen in the use of knowledge discovery and data mining with big data to discover clusters and relationships, as opposed to using a theory and hypothesis to develop a traditional clinical trial, thereby redefining (or at least expanding) the concept of research. Third-level change involves changes at the societal and institutional level, typically occurring over long periods of time. For instance, the evolving role of the nurse from a handmaiden for the physician to a leader in healthcare delivery can be seen as a third-level change.
Today, innovations in healthcare and computer technology are interactively creating first-, second-, and third-level changes, creating the future of healthcare within a society that is also undergoing change at all levels. Informatics experts are among the key leaders managing and guiding these change processes within healthcare. However, they face a number of challenges in achieving these goals.
The Challenge of Anticipating Future Directions
In 1970 Alvin Toffler published the book Future Shock.11 One of the themes in the book was “what happens to people when they are overwhelmed by change. It is about how we adapt or fail to adapt to the future.”11(p1) Interestingly, Future Shock was written long before the widespread use of personal computers or the Internet. Today innovations in practice and technology are changing healthcare delivery at an ever-increasing speed. As Toffler identified many decades ago in a slower-paced world, for many the degree and speed of change is overwhelming. This includes people in healthcare in the midst of a knowledge explosion who must do more than just adjust to overwhelming change.
While there are no research methods for predicting the future with absolute certainty, techniques can be used to rationally predict future directions and trends. A historical example of this is the publication of the book Megatrends by John Naisbitt in 1982, well before the general population was even aware of the Internet or the potential of owning a computer. Megatrends are trends that affect all aspects of society. The 10 trends identified by Naisbitt are listed in Box 31-3. These trends, identified many years ago, continue to have a major influence on health informatics today.
While health informatics specialists clearly recognize the importance of planning and the long-term implications of building today's healthcare information systems, there are immediate challenges in thinking about the future. First, present issues are often more pressing and take a higher priority over tasks that can wait for another day. This type of thinking is sometimes referred to as “putting out fires.” For example, a health informatics specialist may spend an afternoon answering users' questions but as the number of communications increases, the notes documenting these calls can become increasingly sparse. Trends and patterns that could be used as a basis for a new education and training program, or for upgrading functions in the current healthcare informatics system, can be lost in the pressing demands of the moment.
Box 31-3 Naisbitt's Megatrends for the 1980s
Industrial society → Information society
Forced technology → High tech/High touch
National economy → World economy
Short term → Long term
Centralized → Decentralized
Institutional help → Self-help
Representative democracy → Participatory democracy
Hierarchies → Networking
North → South
Either/Or → Multiple options
Second, small rates of growth often seem insignificant. However, major trends start from small, persistent rates of growth. This is especially true when dealing with exponential growth. A few years ago very few patients asked for copies of their health reports and a very small percentage of those patients would have considered accessing their healthcare data via the Internet. In August 2012 the Veterans Health Administration (VHA) reported that the one millionth patient had used the Blue Button application to download data from his or her personal health record (PHR).12
Third, there are intellectual, imaginative, and emotional limits to the amount of change that individuals and organizations can anticipate. The imagined future is built on assumptions developed in the past and therefore includes gaps and misinterpretations. Future predications can seem vague and the farther one looks into the future, the more disconnect there is between the present and the significance of the future. For example, nurses educated in small diploma schools 50 years ago usually called a physician to restart an intravenous (IV). Nurses from that time period would have struggled to anticipate the high levels of responsibility common in today's staff nursing role.
Approaches for Predicting
Qualitative and quantitative methods are used in traditional forecasting and planning as well as by futurists to foresee, manage, and create the future. The use of established research methods separates these researchers from soothsayers. Multiple methods used in concert are needed to identify and address future challenges. Selected examples of these methods are presented here. In addition, Box 31-4 includes resources for exploring a number of other methodologies used in this field of study.
Trend Analysis and Extrapolation
Trend analysis involves looking at historical data and identifying trends over time in those data. For example, a log of help desk calls may demonstrate that over the past 2 months there has been an increasing number of calls from clinical managers and department heads concerning the institution's newly introduced budget software. The new software offers a number of options and levels of analysis that were not used in the past and it is more robust and complex. Initially there were several calls from three managers who work in the same division. However, these managers are now making very few calls. Instead, the majority of the calls are coming from a different division. Extrapolation consists of extending these historical data into the future. For example, if the trend line is sloping upward, one would continue this line at the same degree of slope into future time periods. Needless to say, this historical upward trend line will not continue forever. Eventually the growth will start to slow and an S curve will develop. With an S curve the growth is slow initially but then becomes very rapid. Once the event begins to reach its natural limit the rate of growth slows again.
A potential example of this pattern is the future use of PHRs by the general public. Initially only a small number of people were using this resource. Google, an early entrant in PHR development, withdrew from this market because of lack of interest by the general public. However, the current Blue Button data from the VHA suggests that the use of PHRs may be at the beginning of an S curve, with the possibility of very rapid growth in the next few years. The expected patterns of growth can be used to plan educational programming as well as support services. The need for these services can be expected to grow and then level off.
While trend analysis and extrapolation demonstrate using quantitative methods to foresee the future, qualitative methods
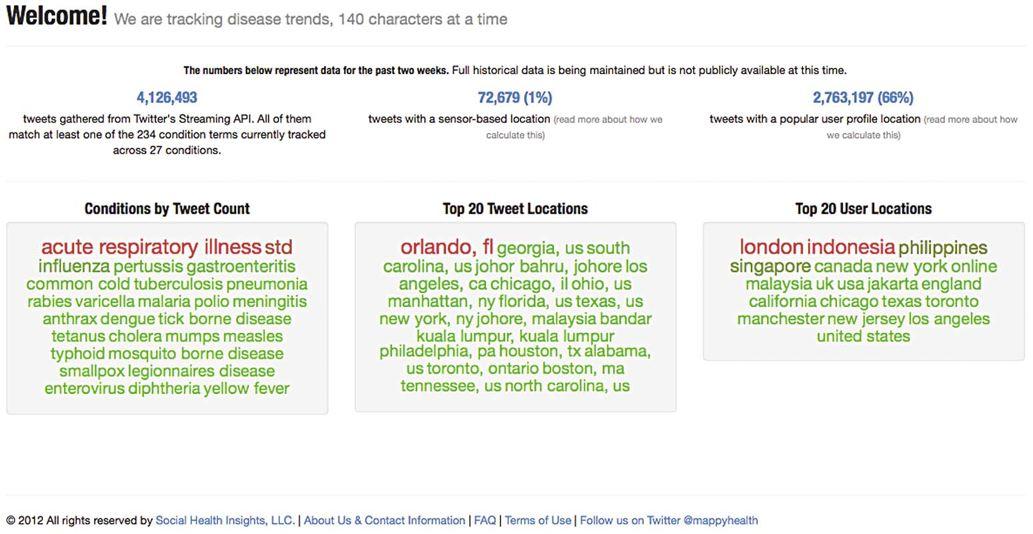
FIG 31-1 MappyHealth home page.
(Copyright Mappyhealth.org.)
are also important. One example of qualitative methods is content analysis.
Box 31-4 Futures Studies Methodologies Resources
• Methods and Approaches of Futures Studies, http://crab.rutgers.edu/~goertzel/futuristmethods.htm
• World Future Society:
• Methods, www.wfs.org/methods
• Methodologies Forum, www.wfs.org/method.htm
• Futures Research Methodology Version 3.0, www.millennium-project.org/millennium/FRM-V3.html
• Five Views of the Future: A Strategic Analysis Framework, www.tfi.com/pubs/w/pdf/5views_wp.pdf
• Methodologies for Studying Change and the Future, www.csudh.edu/global_options/IntroFS.HTML#FSMethodols
Content Analysis
Content analysis was the major research approach used to identify the trends in the book Megatrends. 13 Content analysis within the futures research realm involves reviewing a number of information resources and noting what topics are discussed, what is being said about these topics, and what topics are not discussed. A current example of this type of analysis can be seen in the application MappyHealth (www.mappyhealth.com). MappyHealth uses an automated process to search Twitter posts, looking for trends related to a specific list of diseases. A screenshot showing the types of data being tracked is provided in Figure 31-1. The assumptions made in identifying resources, topics, and trends to monitor can have a major impact on determining the forecasts produced. For example, the initial version of MappyHealth was limited to a list of specific diseases. This is one of the reasons why it is important that informatics specialists review several different resources from several different perspectives to analyze trends.
Scenarios
Scenarios involve asking individuals to envision possible futures within a certain context. For example, people may be asked to describe the EHR one might expect to see 10 to 15 years in the future. This can be done as a group process or individually. Participants should be encouraged to envision scenarios that are multifaceted and holistic, internally consistent, and free of personal bias. Elements in the scenario should not be contradictory or improbable. A well-constructed scenario may suggest events and conditions not presently being considered.
The following three major approaches can be used to construct a scenario:
1.The Delphi method can be used to elicit expert forecasts for a specific time frame. A combination or synthesis of opinions is used to develop the scenario.
2.Experts develop scenarios that reflect the viewpoint of their disciplines. These are modified and combined to produce an overall scenario.
3.A cross-impact technique is used to test the effect of one aspect of the scenario on all of its contributing parts.
The creation of scenarios can be used in concert with backcasting.
Backcasting
With backcasting one envisions a desired future end point and then works backward to determine what activities and policies would be required to achieve that future. Backcasting involves the following six steps:
1.Determine goals or the desired future state
2.Specify objectives and constraints
3.Describe the present system
4.Specify exogenous variables
5.Undertake scenario analysis
6.Undertake impact analysis
The end result of backcasting is to develop alternative images of the future, thoroughly analyzed as to their feasibility and consequences.14
With the rapid changes in informatics, the use of futures research methods is likely to increase. For the first generation of EHRs and data warehouses, informatics specialists have concentrated more on initial implementations than on forecasting future needs. For the next generations of health IT products, futurology can more readily be incorporated in the health informaticist's suite of skills.
Application of Futures Research
The health informatics specialist uses methodologies and strategies from futures studies in two primary ways. First is foreseeing or predicting future trends and directions. For example, in the 1970s and 1980s much of healthcare was financed via fee-for-service funding approaches. Health information systems were designed to capture charges but not to measure the cost of care. A number of items, including nursing and other services, are included in the patient's charge for a hospital room. In a fee-for-service approach, the contribution of each of these items to the total cost was irrelevant. Cost and charges did not need to correlate. The charge could be whatever the market would bear.
The introduction of the prospective payment system in the 1980s and managed care in the 1990s required that healthcare institutions capture costs rather than just charges. Existing information systems were totally ineffective in capturing costs. The ability to predict these kinds of major changes in healthcare delivery could be a significant advantage to vendors and healthcare institutions alike. By predicting the potential costs and benefits, one is better prepared to manage these events. Cost–benefit analysis is an example of using futures studies for management.
Creating the future is the second way in which health informatics specialists use futures studies methods. By thinking of possible futures scenarios, the informatics specialist can work toward creating the environment in which these futures might be possible. By using the work of futurists, as well as applying futures studies tools, it is feasible to imagine possible future trends and directions and thereby work to create preferable future directions.
The Future of Informatics
Health informatics is and will remain a dynamic and complex field. Thus accurately predicting precise directions for the future of health informatics is inherently uncertain. An informal survey of health informatics experts at Medical Informatics Europe 2012 and NI2012 resulted in the following interesting list of projected topics with little overlap (listed in no particular order):
•Robotics
•Cloud computing and “drops from clouds”
•Big data, analytics, and meta-analytics
•Data visualization and information synthesis
•Usability, participatory design, and usability labs
•Augmented reality
•Interprofessional collaboration and cooperation within facilities, across diverse fields inside and outside of informatics, including their implications
•Process modeling with biomedical engineering
•Risk analysis
•eHealth indicators for countries and across nations
•Modularized health informatics systems (available functions or applications versus whole systems)
•Mobile devices for health applications (mhealth)
•Evaluation studies on the impacts of health informatics products
•Personal health, patient-centered health system and applications (moving away from a provider-centered health system), and their implications for informatics
•Ontologies and interoperability, version 2.0
•Health reform and how informatics supports it
•Data reuse for policy-making and decision making
•Theoretical and model-based informatics
•Research-based healthcare using informatics tools
•Increased emphasis on guidelines and protocols to improve care
•EHRs 2.0, redesigned and rethought
•Research and scholarly outlets limited by vendor-support EHRs
•Policy and education role for informaticists15
Formal literature does not provide consensus about emerging or future directions for informatics. Most recently, authors wrote about the future of academic biomedical informatics in 201215; a nursing informatics research agenda for 2008 to 201816; medical informatics past, present, and future in 201017; harnessing information and communication technologies for nurses worldwide in 200818; informatics directions from an IT consulting firm (Table 31-1); and an agenda for nursing informatics in 2006.19 Within informatics and nursing, major past efforts internationally have centered on terminology development.20 Beyond that, a consensus of themes is not apparent across articles and little collaboration to develop future directions across disciplines is evident.
TABLE 31-1 Trends in Healthcare Important to Health IT
TREND
DESCRIPTION
Wellness first
Focus on wellness versus illness
ePower to the patient
Patients take on a larger, more active role in managing their wellness and health
Earlier detection
Earlier detection maximizes options for successful treatment, leading to a speedier return to good health
High-tech healing
New technologies can significantly boost outcomes and quality of life
Resources: more but different
Solving the healthcare resource puzzle requires new players and new care models
Global healthcare ecosystem emerges
More information, more connected, leads to better care and better research.
Adapted from Forum LE. The Future of Healthcare: It's Health, Then Care. Falls Church, VA: Computer Sciences Corporation (CSC); 2010.
Outside the field of healthcare, contemporary issues of The Futurist (www.wfs.org/futurist) list its annual outlook on trends for society. Trends pertinent to healthcare include the following:
•New leader skills. These will be shaped by those with social networking, content management, data mining, and data meaning skills. New job titles include Chief Content Officer and Chief Data Scientist.21
•Nanotechnology products. Buckypaper is composed of industrial-grade carbon nanotubes and is 100 times stronger than steel per unit of weight. It conducts electricity like copper and disperses heat like steel or brass.22
•Nanorobots or nanobots. These carry molecule-sized elements, can detect cancer, and are being developed by researchers at Harvard University.23
•Full-body firewalls. These are necessary to prevent hackers from tampering with wireless medical devices and internal drug delivery systems. Researchers at Purdue and Princeton universities are developing a medical monitor (MedMon) designed to identify potentially malicious activity.24
•Ubiquitous computing environments. Workplaces will become ubiquitous computing environments that include computing capabilities and connectivity.25
•Image-driven communication. Graphics and images will be more heavily relied on for communication, allowing faster comprehension and possibly new ways of thinking but at the cost of eloquence and precision.26
•Living data. Connectivity will expand to millions of things and sensors will gather more data that will be processed by more computers. Data may become too big, so channeling the power of data will become important.27
•The intelligent “cloud.” This will become not just a place to store data but will evolve into an active resource providing analysis and contextual advice.28
Due to the lack of consensus on trends, this chapter weaves threads from available publications, chapter authors' thoughts, and other current informatics perspectives into the following five major themes:
•Consumerism and informatics
•EHRs 2.0
•Usability and improving the user experience for health IT
•Big data and data visualization
•Nanotechnology and nanoinformatics
A substantial part of the chapter is devoted to nanotechnology and nanoinformatics because the topic is likely new to most readers. Also, given its potential impact on society and funding largess in the billions of dollars worldwide, nanotechnology is currently underemphasized in health education and health informatics.
Consumerism and Informatics
A shift is occurring away from provider-centric care toward patient-centered or consumer-centered care.19,21,29 Through current informatics tools, consumers are being supported as they assume more responsibility for their own care, especially those consumers with chronic diseases. The importance of this shift is underscored in several chapters of this book: Chapter 8 (telehealth), Chapter 9 (home health), Chapter 13 (the evolving epatient), Chapter 14 (social media and social networking), and Chapter 15 (PHRs). This future direction is clear and will only grow over time. For example, the design of tailored, mhealth (mobile health) PHRs could include the following:
•Theory-based studies on the impact of consumer health IT products
•The integration of consumer and provider health IT products to increase care collaboration
EHRs 2.0
Clearly, the billions of dollars in Health Information Technology for Economic and Clinical Health (HITECH) Act funding directed at healthcare provider incentives will drive development of future EHRs and correlated topics of interoperability and impact. The HITECH Act funding will continue to increase the number of implemented EHRs, especially among eligible professionals and ambulatory practices, the main target for the HITECH Act funds. What is less clear is how these systems will affect the quality of care and the practice of healthcare. There has been a rush to implement EHRs and attend to Meaningful Use to receive financial incentives. Healthcare providers and sites could easily experience detrimental impacts to workflow and patient care, especially initially, instead of the projected benefits of EHRs. The HITECH Act did not include funding for research to assess EHR impacts,15 so this kind of evaluative research constitutes a future direction for informatics practice as well as needed informatics research. In fact, Shortliffe15 claims that future academics in informatics will find this kind of research one of the only research avenues available to them for EHR-related activities.
Clinicians are disgruntled with the current offerings from EHR vendors. In an editorial for The New England Journal of Medicine, Mandl and Kohane argue that EHR vendors propagate a myth of complexity that precludes innovation and a myth that EHRs are different than more flexible and robust consumer technology.30 With most sites using vendor-supported EHRs, this kind of impatience from users will likely drive important changes for EHR offerings. One change might be that vendors no longer are full-service providers of EHRs. Instead, they may become smaller service and application providers, allowing sites to pick and choose best options among vendors, including nontraditional vendors such as Google or Microsoft.
Newer infrastructure, such as cloud computing, middleware, and mobile applications, could allow more robust integration efforts at the healthcare provider and consumer end of computing. Consumer demand may force EHR vendors to incorporate newer tools in their offerings, such as more robust clinical documentation tools with integrated graphics and drawing capabilities and even a basic spell-checker, which is currently lacking in today's EHRs. Mandl and Kohane indicate that disruptive technologies for EHRs are needed to displace the current model of EHRs. This suggests another future direction for EHRs.
Interoperability efforts will continue, especially in the U.S., where the diversity of products and EHR components has caused the nation to lag behind others in creating integrated, national, longitudinal patient EHRs. Regional integration efforts have helped in the effort to share data. Interoperability beyond regions will be a continued, costly future direction for the U.S. No doubt informatics research and operational efforts on ontologies will continue to facilitate this work, although efforts have been ongoing for decades. What is needed is consensus about ontologies, especially for nursing.
As EHR implementations increase, it is possible that the traditional view of EHRs may fade. EHRs may be less organization- and site-specific, becoming dispersed with data owners related to roles (patient, healthcare provider, insurer, lab, pharmacy, etc.) and data pulled and integrated from geographic or other defined areas. A particular need for the future is more interdisciplinary views and collaborations for EHRs. Given the importance of teams in healthcare, the next generation of EHRs, no matter how they are instantiated, should offer collaborative workflow tools and methods for synthesizing data and information for “at-a-glance” views across disciplines, sites, types of agencies, and traditional EHR modules.
Potential areas for future research include the following:
•Evaluative research on the impacts of EHRs from various viewpoints of patients, healthcare providers, teams, care outcomes, and quality of care
•Impacts of integrative views of patient-centered data across traditional EHR modules and disciplines
•Cost-effectiveness research and comparative effectiveness for EHR designs
Usability and Improving the User Experience for Health IT
In the U.S., recent efforts will likely ensure that improving the user experience is a future trend in health IT. As noted in Chapter 21, two federal agencies are currently involved in EHR usability initiatives: the National Institute of Standards and Technology and the Office of the National Coordinator for Health Information Technology, whose Meaningful Use Stage 2 language includes a section on EHR usability. In June 2012 the Food and Drug Administration released draft language called “Applying Human Factors and Usability Engineering to Optimize Medical Device Design,” available at www.fda.gov/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/ucm259748.htm. These kinds of regulations are likely to proliferate in the future and become more stringent because of patient safety issues.
Given healthcare provider and consumer voices, health IT usability is a much needed future trend. Federal requirements will continue to expand and vendors will have to respond to the need for improved products. Organizations will need to increase their knowledge about and skills for improving the user experience. An excellent resource for meeting this challenge is the Healthcare Information and Management Systems Society (HIMSS) Usability Maturity Model.31 Additional information on this model can be found at HIMSS.org by searching the terms usability and maturity.
Research directions for improving the user experience are many. Examples include the following:
•Comparative effectiveness research on EHR and device designs, especially for complex patient views, such as clinical summaries, care transitions, and Electronic Medication Administration Records (eMARs).
•Developing and implementing best design practices agnostic of vendors. Perhaps decoupling user views from underlying code could occur so that optimal designs could be downloaded by healthcare providers and layered onto their local data.
•Determining outcomes for varying application designs. For instance, improved displays can positively affect clinicians' situation awareness and performance in intensive care units (ICUs).32–34 Similar studies for other applications could be completed.
Big Data and Data Visualization
The term big data was initially defined in 2000 by Francis Diebold, an economist at the University of Pennsylvania (see his paper at http://utpl.academia.edu/nopiedra/Papers/1316242/Big_DataDynamic_Factor_Models_for_Macroeconomic_Measurement_and_Forecasting). Big data resulted from vast quantities of available data due to advances in storage technology. Initially downplayed as ambiguous, the term became popular after an October 2010 information management conference featuring IBM and Oracle.35 For health practitioners the important concept is that huge amounts of data are being generated and relatively inexpensive storage technology will make them even more available in the future.
No matter what term is used, the world is generating mass amounts of data. IBM estimates that 2.5 quintillion bytes of information are generated each day. That is three times the equivalent of the Library of Congress each second.36 In the life sciences, genomic data have created large datasets for analyses. Biomedical informatics efforts are underway to integrate data across disparate fields. For example, the National Center for Integrative Biomedical Informatics from the National Institutes of Health is developing interactive, integrated, analytic, and modeling technologies from molecular biology, experimental data, and published literature.37
Within healthcare, local data warehouses combine longitudinal EHR, administration, and financial data into a searchable database. Sensor data and input from mobile and remote technologies could be integrated with EHR data in the near future. Personalized medicine efforts and nanotechnology promise the expansion of these kinds of databases. Regional efforts and interoperability will also add to the amount of available data. Healthcare providers and informaticists will become familiar with the term big data and using big data will become a reality.
With large datasets an unparalleled opportunity exists to examine data and issues across thousands of data points and patients for data integrated across fields (population data, genomics, etc). However, current efforts are hampered by issues in data quality, missing clinical concepts, lack of standard terminology, and the need for specialized tools.
Analytics
One of the pressing issues with big data is making sense of vast amounts of stored data. Chapter 4 discussed one method for achieving this goal—knowledge discovery and data mining—but others are available, including analytics. The goal of data analytics is to understand big data, develop predictive models, and discover new insights. Analytics help in sense making by revealing patterns in the dataset. Figure 31-2 provides an example from biology and computer science. At the intersection of science, design, and data, data visualization involves understanding principles of human perception, design, and computing capabilities.38
In the life sciences, interdisciplinary teams of biologists and computer scientists developed interactive visualization tools like MulteeSum to compare genes in fruit flies.39 In healthcare, analytic tools for searching data warehouses are emerging and are called business intelligence tools. Because analyzing data and making conclusions from stored data can affect organizational and patient care decisions, the data visualization effort will be an important future trend.
Many analytic tools are available in the marketplace to assist healthcare practitioners. See, for example, a white paper by Gartner Consulting that compares currently available tools at http://www.qlikview.com/us/explore/resources/analyst-reports/gartner-magic-quadrant-business-intelligence-bi-platform.
Research directions for big data and analytic tools include the following:
•Developing interactive visualization tools for health practitioners, especially for nursing, pharmacy, and those less often emphasized
•Developing big data sets combining published literature, population data, and regional data warehouses
•Detecting patterns for interventions and outcomes in regional data warehouses
Nanotechnology
The statement “Big things come in small packages” is appropriate to the field of nanotechnology. Nanotechnology is the study of controlling and altering matter at the atomic or molecular level.40 The focus of the field is the creation of materials, devices, and other structures at the nanoscale (1 to 1000 nm). The produced items are referred to as nanomaterials, which are composed of smaller subunits called nanoparticles. Nanotechnology is a diverse field that requires a collaborative environment across multiple domains (e.g., surface engineering, physics, organic chemistry, molecular biology, and materials science).
History of Nanotechnology
Even though the majority of research in the field of nanotechnology has been conducted in the past few decades, the field began in 1959 when Richard P. Feynman presented a lecture titled “There's Plenty of Room at the Bottom.”41 In this talk he discussed being able to manipulate individual atoms, which would allow for more flexibility and use in synthetic chemistry.
The field expanded in the 1980s with the invention of the scanning tunneling microscope and the discovery of fullerenes. With the scanning tunneling microscope, scientists could visualize particles at the nanoscale. In 1985 Harry Kroto and his collaborators discovered a molecule composed solely of carbon, which they named Buckminsterfullerene.42 Buckminsterfullerene is a spherical molecule composed of 60 carbon atoms. This gives the molecule a high structural integrity and makes it very stable. This discovery laid the foundation for the development of one of the most well-recognized nanoparticles, the carbon nanotube. A carbon nanotube is a nanoparticle composed of carbon atoms bound to one another to form a tubelike structure (Fig. 31-3). Carbon nanotubes are a member of the fullerene family of molecules. They have a unique combination of thermal conductivity, mechanical properties, and electrical properties

FIG 31-2 Example of visualization tools used to compare fruit fly attributes.
(From Fowlkes CC, Eckenrode KB, Bragdon MD, et al. A conserved developmental patterning network produces quantitatively different output in multiple species of Drosophila. PLoS Genet. 2011;7[10]:e1002346.)
that makes them useful in the development of structural materials.
Nanofabrication and Nanomedicine
Nanomaterials and nanoparticles are used in electronics, biomaterials, and healthcare. Some claim that this area of science and technology has the opportunity to revolutionize our world. Manipulation of particles at the nanoscale allows the creation of unique materials with special properties (e.g., unique chemical, physical, or biologic properties, such as increased electrical conductivity or strength). The special properties are due to the particles' incredibly small size, which allows absorption or unique movement, and also due to increased surface areas that interact with their environments, creating increased interactions of materials.
Nanofabrication.
Nanofabrication is the development of materials used in structures, electronics, and commercial products. Fabricated nanoparticles are typically added to larger physical structures to enhance them, resulting in increased strength, elasticity, conductivity, or antimicrobial properties. Much work has been done with carbon nanotubes because the tubelike structure provides increased material strength. Carbon nanotubes are now commonly used in electronics as wiring for electrical components. For example, a research group at Rice University bound carbon nanotubes to Kevlar fibers to make durable, conductive wires that can be used in wearable electronics and battery-heated body armor.43 Quantum dots, whose elements move in all three dimensions, are another nanoparticle often used in electronics as semiconductors.
The number of commercially available items containing nanoparticles has increased at an aggressive pace over the past two decades. When the Project on Emerging Nanotechnologies (PEN) began its inventory in 2006, 212 products were listed. Now PEN estimates that more than 1300 manufactured, nanotechnology-enabled products have entered the commercial marketplace around the world.44 Items containing nanoparticles are very diverse, ranging from everyday items such as nonstick cookware and lotions to unique items such as self-cleaning window treatments. Probably the most commonly used and commercially available product is silver nanoparticles, due to its antimicrobial properties.
Nanomedicine.
Nanomedicine centers on the application of nanoparticles and nanoscience techniques to healthcare and clinical research.45 Its primary goal is the use of nanotechnology for the diagnosis, treatment, and prevention of diseases. Applications include nanoparticles as delivery devices for pharmaceutics, diagnostic devices, and tissue replacement.46 Due to their size and design, nanoparticles behave differently than traditional particles since they avoid the body's immune defense mechanisms, avoid filtration by the body, and interact more with tissues. Antibodies and a variety of other surface-engineered materials can be conjugated to

FIG 31-3 A carbon nanotube.
(Copyright Owen Thomas/123RF Stock Photo.)
the surface of nanoparticles, increasing their specificity for individual cell types (e.g., tumors). Importantly, the use of nanomaterials reduces medication dosages and effects on nontargeted tissues. Current research focuses on exploiting the highly soluble, targeting properties of nanoparticles to improve the delivery of cancer drugs to tumor-containing tissues47 and on using nanoparticles to deliver nonviral genes and small interfering ribonucleic acid (RNA) to combat viruses and cancer.48
Another very intriguing area of nanomedicine research is advanced imaging and thermotherapy. Quantum dot nanoparticles are used in conjunction with magnetic resonance imaging (MRI) techniques to produce exceptional images of tumorous tissues. Chemical or physical groups can be attached to these nanoparticles via surface engineering, so that they seek out tumor cells and increase the resolution of images.49 These same nanoparticles can then be used in the treatment of tumor cells using techniques such as thermotherapy. The process aggregates nanoparticles in tumorous tissues and then excites the nanoparticles using targeted radio waves, lasers, or focused magnetic waves. The excitation causes the metals in these nanoparticles to heat up, raising the temperature of nearby tissues (localized hyperthermia) and causing targeted cell death.50
Work is being done to develop in vitro early detection methods using nanoparticles. Thus nanoparticles are being used as diagnostic tools. One example is the use of a dime-sized microfluidic device containing a network of carbon nanotubes coated with tumor-specific antibodies.51 A patient's blood sample passes through the device and any tumor cells are bound to the nanotubes. Another sensor includes chips containing thousands of nanowires able to detect proteins and other biomarkers produced by cancerous cells. These types of advances could, in the future, enable the widespread detection and diagnosis of cancer in very early stages.
Cautions about Nanotechnology
Even though nanoparticles are incredibly effective and useful, caution is warranted. Unintended consequences of nanomaterials are due to secondary effects, such as cytotoxicity. For the same reasons that nanoparticles are effective (i.e., their size and increased surface interactions), they also can cause toxicity to the environment and humans. This is a key area of concern and current research in the nanoscience and nanomedicine community.52,53 Many authors discuss inherent toxicity due to nanomaterials' cationic surface charge.52–55 This surface charge is necessary for cellular uptake. If the charge is too high, it can create holes within the cell membranes, resulting in membrane degradation, erosion, and ultimately cell lysis. Clearance of nanoparticles from the human body is another key area of concern because nanoparticles may be rapidly eliminated by the kidneys or, alternatively, remain in circulation for long periods of time, increasing exposure and potential toxicity.
Synthetic methods such as the use of surface engineering and biodegradable components to construct nanoparticles are being employed to counteract the inherent toxicity of nanoparticles. These processes are used to alter the cationic surface charge of most nanoparticles by reducing the cationic charge, making it neutral or completely changing it to an anionic charge. However, if the surface charge of nanoparticles is reduced too much, the bioavailability of the nanoparticles is also decreased. Because of potential toxicity, nanoparticles must be evaluated carefully before they are approved for routine use in the clinical arena.55–56
Nanoinformatics
Nanoinformatics was created in an effort to help manage the large volumes of data being produced by the field of nanotechnology. The foundations for nanoinformatics began in 2007 by the U.S. National Science Foundation.57 The focus of nanoinformatics is the use of biomedical informatics techniques and tools for nanoparticle data and information. In October 2011 the U.S. National Nanotechnology Initiative (NNI) document was developed, which outlined the following three major goals for nanoinformatics:
1.Enhance the quality and availability of data about nanoparticles
2.Expand nanotechnology theory, modeling, and simulation
3.Develop an informatics infrastructure58
The first goal has received the most attention to date. A number of groups are standardizing nanotechnology terms and developing ontologies to represent the relationships between the terms. The two most recognized standards organizations in nanotechnology are the Nanotechnology Standards Panel of the American National Standards Institute and the Nanotechnology Technical Committee of the International Organization for Standardization. The National Cancer Institute leads one of the most well-recognized ontology programs in nanotechnology, the NanoParticle Ontology.
Some progress has been made on the second and third NNI goals. The U.S. National Science Foundation hosts a site named nanoHUB that offers a wide variety of nanotechnology simulation tools for use by the general public and researchers. Overall, good progress has been made in the young field of nanoinformatics. However, the future will include much more work in this area.
In the future, one of the most pressing goals is to create an available public database of easily computable, nanoparticle data. To accomplish this, the extensive available literature on nanoparticles needs to be mined for relevant properties matched to existing standards systems or ontologies. This kind of database could then be used for future data mining and model development. Beyond that, a next goal could be to develop predictive modeling software for developing quantitative structure activity relationships for nanoparticles. This would allow researchers to develop computer-generated structural images of nanoparticles and test them in a simulated environment, allowing toxicity predictions and estimates of bioavailability.
Issues in Regulation and Ethics
Authors are debating the regulatory and ethical implications of nanomaterials because of the unique properties and potential toxicity inherent in these materials. While some indicate that current frameworks are adequate to allow regulatory and ethical assessments,59,60 pressing considerations are evident. For example, current cosmetic products such as sunscreens are seldom labeled as containing nanomaterials,61,62 leaving consumers uninformed. No regulations require such labeling as yet.
Scientists can manufacture completely new materials with nanoscience yet reliable information about the safety of nanomaterials lags behind their fabrication.62 Exact risks for patients, employees, and scientists are not yet known. The potential applications for nanomaterials are enormous; likewise, their risks and regulatory and ethical implications are equally grand. Future applications could enhance oxygen storage in blood. This would, of course, be a boon to patients with emphysema but it has implications for ethics and regulation of sports competitions, as well as general use in humans.63 More alarming findings are emerging. For instance, researchers found that nanoparticle uptake by salmon negatively altered feeding behavior and lipid metabolism.64 This finding is of particular concern because this kind of nanoparticle ingestion mimics typical feeding activity in the food chain. Whether regulatory controls will keep pace with discoveries such as these is an issue.
Once nanomaterials are more commonplace in healthcare, ethical issues arise for the workplace related to hazards, risks, and projected controls.65 Ethically, workers will need to be informed about potential exposure to nanomaterials and risks related to inhalation, skin absorption, or unintended ingestion. This implies a responsibility for accurate assessment by employers, communication about risks, and perhaps even a form of informed consent by workers. For patients, expanded informed consent may be needed for nano-based medications because all interactions are unlikely to be identified during testing.46,66 Clearly, safety, regulatory, and ethical concerns are paramount for nanomaterials.
The field of nanotechnology is exciting but caution is warranted. By virtue of the rapid advancements, nanotechnology is a major future direction for informatics, informatics research, commercial product development, health products, and impact assessment.
Conclusion and Future Directions
Health informatics specialists and leaders cannot afford to leave the future to chance. They must proactively and systematically identify future trends and directions in society, healthcare, technology, and informatics. This information and knowledge can provide the foundation for designing and building the health information systems of the future. The methods and trends discussed in this chapter provide tools and thoughts for health informaticists to use to identify important trends locally and regionally.
Acknowledgement: David E. Jones's contribution was supported by Grant Number T15LM007124 from the National Library of Medicine.
References
1.
Centers for Medicare & Medicaid Services: National Health Expenditure Projections 2009–2019. 2009, Centers for Medicare & Medicaid Services, Baltimore, MD.
2.
World Health Organization (WHO): What are the public health implications of global ageing?. 2011, WHO, Accessed October 15, 2012 http://www.who.int/features/qa/42/en/index.html.
3.
Pellerin, C: Global causes of death move from infectious to chronic diseases. June 12, 2008, America.gov, Accessed January 7, 2013 http://www.america.gov/st/health-english/2008/June/20080612141457lcnirellep0.7136347.html.
4.
Wild, S, Roglic, G, Green, A, Sicree, R, King, H: Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 27(5), 2004, 1047–1053.
5.
American Association of Colleges of Nursing (AACN): Nursing shortage. August 6, 2012, AACN, Accessed October 15, 2012 http://www.aacn.nche.edu/media/FactSheets/NursingShortage.htm.
6.
Association of American Medical Colleges: The complexities of physician supply and demand: projections through 2025. 2008, Texas Healthcare Trustees, Accessed October 15, 2012 http://www.tht.org/education/resources/AAMC.pdf.
7.
HealthReform.gov: Fact sheet: The Affordable Care Act. 2010, HealthReform.gov, Accessed October 15, 2012 http://healthreform.gov/newsroom/new_patients_bill_of_rights.html.
8.
Institute for Futures Studies and Knowledge Management, EBS Business School: http://www.ebs.edu/11866.html?&L=1.
9.
Nordlund, G: Time-scales in futures research and forecasting. Futures. 44(4), 2012, 408–414.
10.
Nelson, R: Future directions in health care informatics. In Nelson, SER (Ed.): Health Informatics: An Interdisciplinary Approach. 2002, Mosby, St. Louis, 505–518.
11.
Toffler, T: Future Shock. 1970, Bantam Books, New York, NY.
12.
U.S. Department of Veterans Affairs (VA): Blue Button: download my data. 2012, VA, http://www.va.gov/bluebutton/.
13.
Naisbitt, J: Megatrends. 1982, Warner Communication Company, New York.
14.
Goertzel T. Methods and approaches of future studies. Camden Computing Services, Rutgers Camden. http://crab.rutgers.edu/~goertzel/futuristmethods.htm, n.d.
15.
Shortliffe, EH: The future of biomedical informatics: a perspective from academia. Stud Health Technol Inform. 180, 2012, 19–24.
16.
Bakken, S, Stone, PW, Larson, EL: A nursing informatics research agenda for 2008–18: contextual influences and key components. Nurs Outlook. 60(5), 2012, 280–288, e283.
17.
Haux, R: Medical informatics: past, present, future. Int J Med Inform. 79(9), 2010, 599–610.
18.
Abbott, PA, Coenen, A: Globalization and advances in information and communication technologies: the impact on nursing and health. Nurs Outlook. 56(5), 2008, 238–246, e232.
19.
McCormick, KA, Delaney, CJ, Brennan, PF, et al.: Guideposts to the future—an agenda for nursing informatics. J Am Med Inform Assn. 14(1), 2007, 19–24.
20.
Hovenga, EJ: Milestones of the IMIA-NI history and future directions. St Heal T. 146, 2009, 3–10.
21.
Colon, J: Shakeups in the “C suite”: hail to the new chiefs. The Futurist. 46(4), 2012, 6–7.
22.
Bisk, T: Unlimiting energy's growth. The Futurist. 46(3), 2012, 31.
23.
World Future Society: World trends & forecasts. The Futurist. 46(3), 2012, 15–16.
24.
World Future Society: Blocking bodyhackers. The Futurist. 46(4), 2012, 2.
25.
World Future Society: The best predictions of 2011. The Futurist. 46(1), 2012, 30.
26.
Baines, L: A future of fewer words?: five trends shaping the future of language. The Futurist. 46(2), 2012, 46.
27.
Johnson, BD: The secret life of data in the year 2020. The Futurist. 46(4), 2012, 21–23.
28.
Carbone, C, Nauth, K: From smart house to networked home. The Futurist. 46(4), 2012, 30.
29.
Forum, LE: The Future of Healthcare: It's Health, Then Care. 2010, Computer Sciences Corporation, Falls Church, VA.
30.
Mandl, KD, Kohane, IS: Escaping the EHR trap—the future of health IT. New Engl J Med. 366(24), 2012, 2240–2242.
31.
Healthcare Information and Management Systems Society (HIMSS): Promoting Usability in Health Organizations: Initial Steps and Progress toward a Healthcare Usability Maturity Model. 2011, HIMSS, Chicago, IL.
32.
Koch, SH, Weir, C, Haar, M, et al.: Intensive care unit nurses’ information needs and recommendations for integrated displays to improve nurses’ situation awareness. J Am Med Inform Assn. 19(4), 2012, 583–590.
33.
Gorges, M, Staggers, N: Evaluations of physiological monitoring displays: a systematic review. J Clin Monit Comput. 22(1), 2008, 45–66.
34.
Drews, FA, Westenskow, DR: The right picture is worth a thousand numbers: data displays in anesthesia. Hum Factors. 48(1), 2006, 59–71.
35.
McBurney, V: The origin and growth of big data buzz. 2012, Toolbox for IT/Topics/Business Intelligence/Blogs, Available from Accessed January 16, 2013 http://it.toolbox.com/blogs/infosphere/the-origin-and-growth-of-big-data-buzz-51509.
36.
Silver, N: The weatherman is not a moron. The New York Times. September 9, 2012.
37.
Athey, BD, Cavalcoli, JD, Jagadish, HV, et al.: The NIH National Center for Integrative Biomedical Informatics (NCIBI). J Am Med Inform Assn. 19(2), 2012, 166–170.
38.
Meyer, M: Visualizing data: why an (interactive) picture is worth 1000 numbers. Gould lecture series: technology and the quality of life. September 5, 2012, University of Utah.
39.
Meyer, M, Munzner, T, DePace, A, Pfister, H: MulteeSum: a tool for comparative spatial and temporal gene expression data. IEEE Trans Vis Comput Graph. 16(6), 2010, 908–917.
40.
National Nanotechnology Initiative: What is nanotechnology?. 2012, Nano.gov, http://www.nano.gov/nanotech-101/what/definition.
41.
Feynman, RP: There's plenty of room at the bottom. Caltech Engineering and Science. 23(5), 1960, 22–36.
42.
Kroto, HW, Heath, JR, O'Brien, SC, Curl, RF, Smalley, RE: C60: buckminsterfullerene. Nature. 318(6042), 1985, 162–163.
43.
Xiang, C, Lu, W, Zhu, Y, et al.: Carbon nanotube and graphene nanoribbon-coated conductive Kevlar fibers. ACS Appl Mater Interfaces. 4(1), 2012, 131–136.
44.
The Project on Emerging Nanotechnologies (PEN): Nanotech-enabled consumer products continue to rise. 2012, PEN, http://www.nanotechproject.org/news/archive/9231/.
45.
de la Iglesia, D, Maojo, V, Chiesa, S, et al.: International efforts in nanoinformatics research applied to nanomedicine. Methods Inf Med. 50(1), 2011, 84–95.
46.
Staggers, N, McCasky, T, Brazelton, N, Kennedy, R: Nanotechnology: the coming revolution and its implications for consumers, clinicians, and informatics. Nurs Outlook. 56(5), 2008, 268–274.
47.
Zhao, P, Wang, H, Yu, M, et al.: Paclitaxel loaded folic acid targeted nanoparticles of mixed lipid-shell and polymer-core: in vitro and in vivo evaluation. Eur J Pharm Biopharm. 81(2), 2012, 248–256.
48.
Zhou, J, Liu, J, Cheng, CJ, et al.: Biodegradable poly(amine-co-terpolymers for targeted gene delivery. Nat Mate. 11(1), 2012, 82–90.
49.
Pericleous, P, Gazouli, M, Lyberopoulou, A, Rizos, S, Nikiteas, N, Efstathopoulos, EP: Quantum dots hold promise for early cancer imaging and detection. Int J Cancer. 131(3), 2012, 519–528.
50.
Ma, M, Chen, H, Chen, Y, et al.: Au capped magnetic core/mesoporous silica shell nanoparticles for combined photothermo-/chemo-therapy and multimodal imaging. Biomaterials. 33(3), 2012, 989–998.
51.
Veetil, JV, Ye, K: Development of immunosensors using carbon nanotubes. Biotechnol Prog. 23(3), 2007, 517–531.
52.
Elsaesser, A, Howard, CV: Toxicology of nanoparticles. Adv Drug Deliv Rev. 64(2), 2012, 129–137.
53.
Fadeel, B, Garcia-Bennett, AE: Better safe than sorry: understanding the toxicological properties of inorganic nanoparticles manufactured for biomedical applications. Adv Drug Deliv Rev. 62(3), 2010, 362–374.
54.
Mukherjee, SP, Davoren, M, Byrne, HJ: In vitro mammalian cytotoxicological study of PAMAM dendrimers—Towards quantitative structure activity relationships. Toxicol In Vitro. 24(1), 2010, 169–177.
55.
Adiseshaiah, PP, Hall, JB, McNeil, SE: Nanomaterial standards for efficacy and toxicity assessment. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2(1), 2010, 99–112.
56.
Blobel, B: Architectural approach to ehealth for enabling paradigm changes in health. Methods Inf Med. 49(2), 2010, 123–134.
57.
U.S. National Science Foundation: Workshop on nanoinformatics strategies http://128.119.56.118/~nnn01/Workshop.html, 2007, Accessed 2012.
58.
National Nanotechnology Initiative (NNI): NNI 2011 Environmental, Health, and Safety Research Strategy October 20, 2011. Available at http://www.nano.gov/node/681, Accessed June 6, 2012.
59.
Litton, P: “Nanoethics”? What's new?. Hastings Cent Rep. 27(1), 2007, 22–27.
60.
Godman, M: But is it unique to nanotechnology?: reframing nanoethics. Sci Eng Ethics. 14(3), 2008, 391–403.
61.
White, GB: Missing the boat on nanoethics. Am J Bioeth. 9(10), 2009, 18–19.
62.
Hristozov, DR, Gottardo, S, Critto, A, Marcomini, A: Risk assessment of engineered nanomaterials: a review of available data and approaches from a regulatory perspective. Nanotoxicology. 6, 2012, 880–898.
63.
Toth-Fejel, T: Nanotechnology will change more than just one thing. Am J Bioeth. 9(10), 2009, 12–13.
64.
Cedervall, T, Hansson, LA, Lard, M, Frohm, B, Linse, S: Food chain transport of nanoparticles affects behaviour and fat metabolism in fish. PLoS One. 7(2), 2012, e32254.
65.
Schulte, PA, Salamanca-Buentello, F: Ethical and scientific issues of nanotechnology in the workplace. Environ Health Perspect. 115(1), 2007, 5–12.
66.
Resnik, DB, Tinkle, SS: Ethical issues in clinical trials involving nanomedicine. Contemp Clin Trials. 28(4), 2007, 433–441.
Discussion Questions
1. In your setting, which future trends are likely to have the largest effect on patient care and related information systems?
2. The 10 trends identified by Naisbitt are listed in Box 31-3. Add two columns to this box. In the first new column project where these trends will be in the next 10 years. In the second new column describe how your projected impact might influence future directions in informatics.
3. Select one of the chapter topics in this book. For example, you might select PHRs in Chapter 15. Use the three levels of change to describe how your selected area of informatics might evolve over the next several years.
4. Use Box 31-4 to access and explore a futures research methodology that was not discussed in this chapter. Describe the methodology and how it could be used in health informatics.
5. Compare and contrast the trends of EHR directions and consumer-centered health informatics. Where do they overlap and where do they differ?
6. Describe how nanomaterials might affect your own life in the near future. Consider the consumer products you use and your role in healthcare.
7. Using futures research methods, identify how you think nanotechnology might impact both health IT and health informatics.
Case Study
You have just been hired as the chief informatics officer (CIO) for a new health system. The health system has 23 acute care facilities and 36 outpatient clinics. It serves as a regional referral center for three states in the Midwest. Your installed base includes a vendor-supplied EHR from a national firm. Work on the data warehouse is just beginning. You have more than 300 varying applications across sites, including everything from a stand-alone pharmacy application for drug interactions to a cancer registry. Your goal is to provide IT support for the organizational vision of being the premier health organization in patient safety for the region. One of the first things you want to do is to plan for the future of IT.
Discussion Questions
1. Given the future directions discussed in this chapter, select the two directions you want to emphasize. Provide rationale for your choices.
2. Discuss how you can use methodologies from futures research to plan for your preferred future with the future directions you selected in Question 1.
3. Outline steps to introduce the chief executive officer to nanotechnology and its potential impact on the organization.
4. You want to increase collaborative work with a local university. What future directions for education do you think are most important as CIO?
Pageburst Integrated Resources
![]()



