Students will: Assess clients presenting for psychotherapy Develop genograms for clients presenting for psychotherapyTo prepare: Select a client whom you have observed or counseled at your practicum
Week 3
Assignment 2: Practicum – Assessing Clients
Name: Amina. H
DOB; 1/10/1987
Age: 32
Gender : Female
Race: Black or African American
Facility: REH Crisis Stabilization Program
City: Minneapolis State: MN
Presenting problem- Excessive alcohol use, Homelessness
History or present illness
Amina is a Somali immigrant that left the war-torn country. She is experiencing an increase in mental health symptoms and stress, especially anxiety and other trauma-related stress. Having difficulty with connecting to other people due to several trauma-related symptoms and Currently homeless. Amina is required by CPS to remain sober and enter treatment in order to maintain custody of her six kids.
Past psychiatric history
Amina has indicated that When under the influence of alcohol, Amina has gotten into fights at times. She is currently not using alcohol, and is requesting to be administered UA's or breathalyzers to verify that she is not using alcohol.
Amina has endorsed racing thoughts and rumination, paranoia/fear, dissociation, difficulty staying asleep, nightmares, negative cognitions of self, others, and the world; crying episodes, depressed mood, heightened startle response, shakiness, and irritability
Medical history
Client denies syncope, lightshades, fever, or numbness or tingling States that her generalized pain is 8/10. administered 400mg of Ibuprofen.
Substance use history
Amina reported that she has had more than 10 years history of over using alcohol, and she seeking to enter Substance use treatment for alcohol
Developmental history
No history available. Patient is an immigrant from Somalia
Family psychiatric history
No history available
History of abuse/trauma
Amina has endorsed persistent worrying that is difficult to control, experience of war, experience of childhood physical abuse,
Review of Systems:
General: Denies fever chills or malaise, Denies weakness or fatigue. Client is alert and oriented to person, place, and time as well as to situation. Client weighs 176 lbs. but client expresses her ideal weight to be 140lbs
Skin, Hair Nails: No problems reported
HEENT- denies a headache, dizziness, or syncope. Denies any hearing issues, denies tinnitus. Denies problems or changes in his vision; denies blurred vision; denies seeing spots.
Cardiovascular: BP 124/104 on left arm sitting and 156/108 on right arm sitting. HR regular and at 97 beats per minute. Denies chest pain and palpitations
Pulmonary: Oxygen saturation 98%. Denies asthma or any other pulmonary disorder. Denies shortness of breath; respirations 16.
Gastrointestinal: Bowel is regular
Genitourinary: Regular urinary pattern
Neurologic: Client informs that she was diagnosed with polio when she was 7. Denies numbness and tingling; or paresthesia
Musculoskeletal– Client informs that she was diagnosed with polio when she was 7. Patient states that she has generalized aches and pains.
Hematology: Denies easy bruising or history of anemia
Endocrine: Denies increase thirst or urination,
Mental Health: Mental status exam
Amina presented cooperative during the clinical interview. Her eye contact is poor. Speech is clear, coherent, but tangential at times. Speaks broken English. She makes no unusual motor movements and demonstrates no tic. Mood was dysphoric. Affect however is restricted. She denies visual or auditory hallucinations. No delusional or paranoid thought processes noted. She is alert and oriented to person, place, and time. She reported that there were six children and she is estranged from them due to her excessive alcohol use. She reported depression and has a noticeable restrained affect, with an occasional smile. She denies visual or auditory hallucination, and her thought process is intact. The client’s awareness is age appropriate and associated with proper judgment and understanding. She denies current suicidal ideation. The diagnostic test of Patient Health Questionnaire-9 (PHQ-9) was administered to the client. The score was 16, which indicates severe depression.
Differential diagnosis
Depression, Post Traumatic Stress Disorder (PTSD), Alcohol Use Disorder
Case formulation
Drawing up from psychiatric viewpoint, the premise of Amina issues may have result from been a witness and experience of war, and extensive childhood physical abuse, and overall the family is not supportive, and lost custody of her children. Her presentation is congruent with reported content.
Treatment plan
Goal #1
Amina will be able to reduce and manage her anxiety
Objective
| Amina will develop her coping skills, and build on her current coping approaches of breathing, prayer, and self-soothing techniques such as taking a walk. |
Intervention
Staff will check in with Amina 2-3 times to assess her practice of coping skills, and to offer information regarding additional coping skills including progressive muscle relaxation, visualization, assertive communication of her feelings.
Goal #2
Amina will attend her therapy sessions
Objective
Amina will continue her sessions with the trauma-informed therapist, with an upcoming appointment next week.
Intervention
Staff will process current feeling about what to expect and how she is feeling about the appointment.
Goal #3
Amina will complete a substance use disorder (SUD) treatment.
Objective
Amina will complete rule 25 assessment to be able to gain admission into treatment center at Park Ave Women's center.
Intervention
Staff will encourage Amina to attend her assessment session and develop a relapse prevention plan.
Genogram
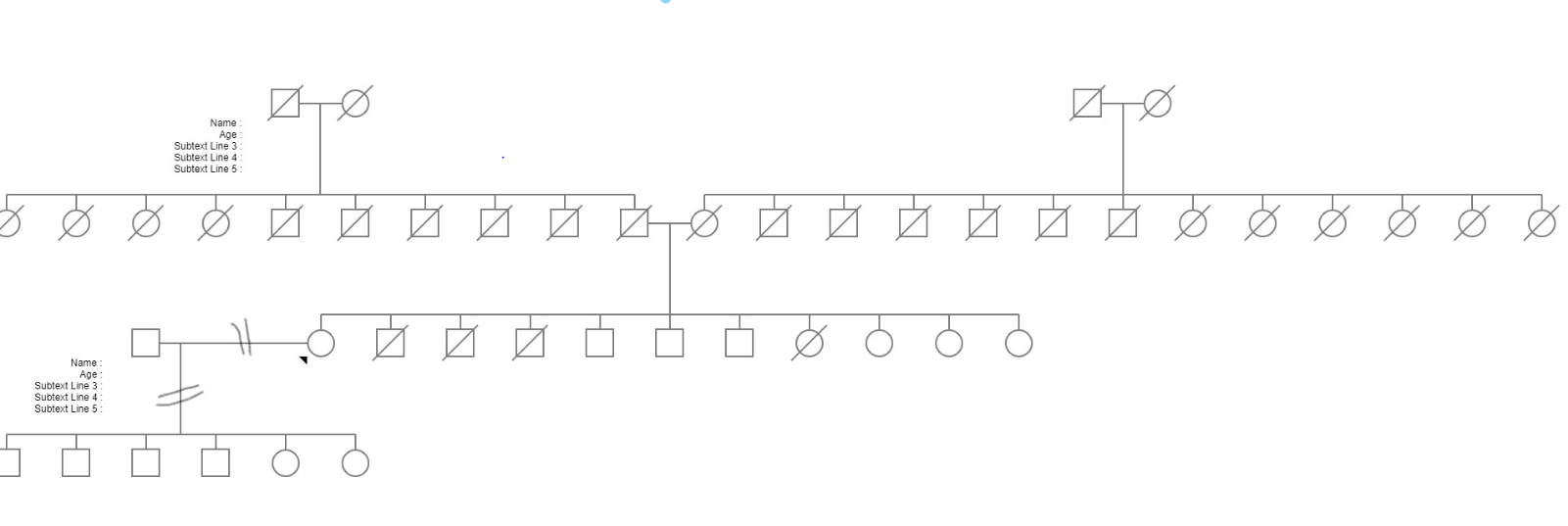
Amina’s children’s ages- 2,3,5, 7,8,9
Amina is estranged from her husband and children
Amina does not have any extended family in the US



