Please see attached
Exam 2
The following 8 questions refer to the scenario for Michelle Owens
Michelle Owens is a 56 year old woman with a new diagnosis of poorly differentiated adenocarcinoma of the colon, The cancer is stage 4 and T2, N2, M1. She is very weak and placed on bedrest. Ms. Owens also has Mitral Valva Prolapse Syndrome (MVPS). Vital signs are: 37.9 C, 82, 20, 128/68, 98% on room air.
Question 1
1 / 1 pts
MVPS results in increased risk of developing which of the following?
Pneumonia
Myocarditis
Endocarditis
Rheumatic fever
Question 2
1 / 1 pts
Ms. Owens' malignant cells are likely to exhibit which of the following?
Increased cellular communication
Low levels of fibronectin
Decreased metabolic demand
Low levels of cachectin
Question 3
1 / 1 pts
Ms. Owens may benefit from antibiotics in which of the following situations?
Never because of resistance
Only after lower gastronintestinal infections develop
Only after upper gastrointestinal infections have resolved
Before surgical procedures
Question 4
1 / 1 pts
Ms. Owens' malignancy development may be promoted by which of the following?
Increased apoptosis
Inactivation of p53 tumor suppressor genes
Decreased angiogenesis
Decreased growth factor receptors
Question 5
1 / 1 pts
MVPS results in which of the following?
Mitral valve not opening properly during ventricular systole
Mitral valve not closing properly during ventricular systole
Mitral valve not opening properly during ventricular diastole
Mitral valve not closing properly during ventricular diastole
Question 6
1 / 1 pts
Ms. Owens' malignancy involves which of the following?
Preinvasive epithelial tumor of glandular origin
Cells that do not closely resemble normal colon cells
No lymph node involvement
Cancer that is only locally invasive
Question 7
1 / 1 pts
MVPS may result in the development of which of the following?
Decreased cardiac output
Acute Pericarditis
Increased cardiac output
Pericardial tamponade
IncorrectQuestion 8
0 / 1 pts
Ms. Owens' malignancy development may be promoted by which of the following?
Telomerase genes in the “switched on” position
Contact inhibition between cells
Density dependent inhibition of cellular growth
Cellular anchorage dependence
The next 4 questions refer to the scenario for Yoobin Chung
Ms. Chung is a 25 year old college student with complaints of fatigue and weight loss these past few months. Today she comes to the student health center with swelling in her left groin and a fever. Ms. Chung has a chest x-ray which reveals hilar lymphadenopathy. Ms. Chung’s legs are pink, warm, and dry, with notable edema of the left leg. Ms. Chung is quite anxious about her health problems and is sobbing uncontrollably, declaring “I don’t want to die”. A needle biopsy of the left groin lymphatic mass reveals lymphoid hyperplasia with Reed-Sternberg Cells.
Vital signs are: 38.2 C, 106, 26, 96/48. 96% sat, Pain 0/10
Question 9
1 / 1 pts
If Ms. Chung's weight loss continues coupled with anorexia & asthenia, this could be related to increased production of which of the following?
Uric acid
Fibronectin
Telomerase
Cachectin
IncorrectQuestion 10
0 / 1 pts
Ms. Chung’s lymphoma would be staged at which of the following?
2a
2b
3a
3b
IncorrectQuestion 11
0 / 1 pts
Which of the following is the likely cause of the left leg swelling?
Decreased hydrostatic pressure
Decreased plasma oncotic pressure
Increased capillary permeability
Obstructed lymphatic drainage
Question 12
1 / 1 pts
Ms. Chung’s malignancy would be classified as which of the following?
Non-Hodgkin’s lymphoma
Multiple Myeloma
Chronic lymphocytic lymphoma
Hodgkin’s lymphoma
The following 5 questions refer to the following scenario for Martin Englewood.
Marion Englewood is a 60year old female with a history of coronary artery disease and primary hypertension. Her medical conditions have been well controlled by medications. She is admitted to the emergency room with acute onset of confusion, pulmonary crackles, nausea and vomiting, and a BP of 212/154.
IncorrectQuestion 13
0 / 1 pts
Which of the following interventions would help to reduce the blood pressure?
Administer fluid
Administer a vasoconstrictor
Block Beta receptors
Administer anticholinergic medications
IncorrectQuestion 14
0 / 1 pts
Ms. Englewood’s hypertension status in the emergency room would be classified as which of the following?
Primary
Secondary
Malignant
Complicated
IncorrectQuestion 15
0 / 1 pts
Select a characteristic of malignant cells that may explain the metastasis of Ms. Englewood’s breast cancer.
Increased Cachectin
Decreased Fibronectin
Decreased angiogenesis factor
Increased Uric Acid
Question 16
1 / 1 pts
Diagnostic tests confirm a diagnosis of metastatic infiltrating ductal carcinoma of the breast. Metastasis to her bones is noted. Ms. Englewood’s malignancy involves malignant transformation of which of the following?
connective tissue
glandular tissue
myeloid tissue
epithelial tissue
Question 17
1 / 1 pts
During physical exam, findings suggestive of breast cancer are discovered. Select the clinical manifestation(s) associated with breast cancer.
Multiple lumps in both breasts
Painful lumps
Dimpling and retraction
Fluctuation in lesion size
The following 7 questions refer to the following scenario for Chris Martin.
Chris Martin is a 29 year old man with cystic fibrosis (CF) admitted to the hospital for a pulmonary infection. He has a barrel chest, dry skin and mucous membranes, clubbing of the nailbeds, dyspnea on exertion, difficulty gaining weight, pedal edema, & steatorrhea.
Mr. Martin is awaiting a lung transplant and hopes donor lungs become available soon.
Vital signs are 38.8C, 108, 26, 98/64. The following laboratory values are obtained:
IncorrectQuestion 18
0 / 1 pts
Mr. Martin has pulmonary hypertension, which places him at high risk for which of the following?
Developing asthma
Developing pulmonary embolism
Developing atelectasis
Developing cor pulmonale
Question 19
1 / 1 pts
Chris’s difficulty gaining weight & steatorrhea are related to which of the following?
Hyperhomocysteinemia and folate deficiency
Obesity- hypoventilation syndrome
Anorexia-cachexia syndrome
Malabsorption
IncorrectQuestion 20
0 / 1 pts
Mr. Martin develops hemoptysis, therefore a sputum for AFB is ordered to rule out which of the following?
Tuberculosis
Pneumocystis carnii pneumonia
Pleurisy
Adenocarcinoma
Question 21
1 / 1 pts
Considering the admission ABG, Mr. Martin should have which of the following?
Not have oxygen administered
Have oxygen administered to increase the SaO2 to >95%
Have oxygen administered to increase the SaO2 to the 88-92% range
Be removed from the lung transplant list because of his physical condition.
IncorrectQuestion 22
0 / 1 pts
A chest x-ray is done revealing a left pneumothorax, therefore a chest tube is placed into the pleural space, which resolves the problem. Mr Martin breathes shallowly however because it hurts. You assess diminished breath sounds and crackles, indicating the likely development of which of the following?
Atelectasis
Dead space units
Congestive heart failure
Alpha 1 antitrypsin deficiency
Question 23
1 / 1 pts
Mr. Martin develops acute hypoxemia, tracheal shift, and hypotension associated with a severe coughing episode, indicating the likely development of which of the following?
Pleurisy
Empyema
Tension pneumothorax
Obstructive pulmonary disease
IncorrectQuestion 24
0 / 1 pts
Mr. Martin’s barrel chest has developed secondary to which of the following?
Acute hypoxemia
Chronic air trapping
Thoracic muscle atrophy
Restrictive pulmonary disease
The following 3 questions refer to the following scenario for Bernie Irving.
Bernie Irving is a 66 year old man who developed an abdominal aortic aneurysm which ruptured in the operating room but was surgically repaired. Mr. Irving’s postoperative course has been complicated with blood pressure issues and respiratory insufficiency. Breath sounds are decreased in the bases with bilateral fine crackles. Mr. Berlin has been smoking for 50 years.
Vital signs are 38.2, 108, 28, 154/96. The following laboratory values are obtained:
IncorrectQuestion 25
0 / 1 pts
Considering the above ABG, Mr. Irving should have which of the following?
Not have oxygen administered
Have oxygen administered to increase the SaO2 to >95%
Have oxygen administered to increase the SaO2 to the 88-92% range
Be admitted to the intensive care unit for acute respiratory failure
IncorrectQuestion 26
0 / 1 pts
Mr. Irving's blood pressure would benefit from which of the following?
Abundant fluid administration
Inotropic medication administration
Anticholinergic medication administration
Alpha blocker medication administration
Question 27
1 / 1 pts
Mr. Irving develops edema, warmth, and pain in his right calf, with strong pedal pulses and a positive Homan’s sign, suggesting that he has developed which of the following?
Acute arterial insufficiency
Deep vein thrombophlebitis
Chronic arterial insufficiency
Varicose veins
The following 6 questions refer to the scenario for Angela Bucaro
Angela Bucaro is a 75 year old retired librarian. Ms. Bucaro smokes two packs of cigarettes a day and says she has tried to quit smoking, but has poor will power. Ms. Bucaro has a long history of coronary artery disease (CAD). She had an anterior wall myocardial infarction (AWMI) several years ago and had a 4 vessel coronary artery bypass graft (CABG). She takes numerous medications, including anti-hypertensives, anti-anginals, diuretics, and anticoagulants. She continues to have periodic episodes of chest pain when she exerts herself too much, but she always gets relief from either rest alone or sometimes requires nitroglycerine. She has a productive cough of green mucous, barrel chest, and bilateral pedal edema.
Vital Signs are 37.8C, 112, 28, and 148/94.
IncorrectQuestion 28
0 / 1 pts
Considering the above data base, Ms. Bucaro’s angina would be classified as which of the following?
Classic angina
Crescendo angina
Unstable angina
Prinzmetal angina
IncorrectQuestion 29
0 / 1 pts
Ms. Bucaro takes several cardiac medications. Which of the following types of medications would benefit her myocardial oxygen and supply balance?
Epinephrine
An anticholinergic
A beta blocker
An alpha adrenergic medication
IncorrectQuestion 30
0 / 1 pts
Ms. Bucaro exhibits which of the following factors that can imbalance her myocardial oxygen supply and demand?
green mucous
bilateral Pedal Edema
barrel Chest
tachycardia
Ms. Bucaro has chest pain that does not respond to rest and nitroglycerine. A 12 lead ECG is ordered and cardiac enzymes are drawn.
IncorrectQuestion 31
0 / 1 pts
Which of the following is true regarding healing of the myocardium after an MI?
A tough inelastic scar develops in 6-12 hours after the MI onset
A weak fibrotic scar forms 2-4 days after the MI onset
Inflammation has its onset approximately 6 days after MI onset
10-14 days after MI onset cardiovascular function improves and she may start feeling better
Question 32
1 / 1 pts
Ms. Bucaro is diagnosed with atrial fibrillation, therefore which of the following is true?
Tachycardia is beneficial
There is an increased risk of stroke
Anticoagulants are contraindicated
Cardiac output is likely to be increased
IncorrectQuestion 33
0 / 1 pts
Which of the following changes would be indicative of myocardial injury?
ST segment depression
T wave inversion
ST segment elevation
P wave depression
The following 5 questions refer to the scenario for Adelaide Hunting
Adelaide Hunting is a 79 year old housewife. Ms. Hunting smokes two packs of cigarettes a day and says she has tried to quit smoking, but has poor will power. She has a productive cough of green mucous, barrel chest, and bilateral pedal edema.
Vital Signs are 37.8C, 112, 28, and 148/94.
Question 34
1 / 1 pts
Which of the following medications may help resolve her blood pressure issues?
A sympathomimetic
A diuretic
An anticholinergic
A vasoconstrictor
IncorrectQuestion 35
0 / 1 pts
A pleural effusion is noted on a chest x-ray, which may result in which of the following?
Compression atelectasis
Pulmonary embolism
Open pneumothorax
Acute obstructive pulmonary disease
Question 36
1 / 1 pts
Ms. Hunting develops acute onset of wheezing, dyspnea, and coughing related to a staff members strong perfume. The wheezing is likely related to which of the following?
Bronchodilation
Elastase production
Bronchospasm
Alpha 1 antitrypsin deficiency
Question 37
1 / 1 pts
Ms. Hunting's breathing difficulty with wheezing and dyspnea may benefit from administration of which of the following?
Bronchodilating medications
Parasympathetic medications
Cholinergic medications
Beta blocking medications
IncorrectQuestion 38
0 / 1 pts
The wheezing subsides. Ms. Hunting declares she has had asthma all her life and that her mother and son have asthma too. She has had positive skin tests and says cats, dust, and perfumes are her triggers. Ms. Hunting’s asthma would be classified which of the following?
Intrinsic
Status asthmaticus
Extrinisic
Non-allergic
The following 7 questions refer to the following scenario for John Fletcher
John Fletcher is a young man with a history of HIV infection who is admitted for fatigue, night sweats, a 20 lb weight loss over the last few months, swollen lymph nodes, and pedal edema. He has a productive cough with yellow/brown mucous & complains of orthopnea. Kaposi Sarcoma was diagnosed last month.
Vital signs are 38.9C 112 30 118/76. Labs are assessed & a physical examination is performed.
CBC Reveals:
RBC, 2.0 mill/mm3, Hgb - 6 gm/dl, HCT -18%
MCV - 108fl (80-97) MCH 29 (27-31), MCHC 34% (32-36)
Platelets - 30,000
WBC - 14,900
Polys - 70%, Bands - 2%, Eos - 2%, Basos - 1%, Blasts 20%, Monos 5%
IncorrectQuestion 39
0 / 1 pts
Mr. Fletcher's pedal edema is related to which of the following?
increased hydrostatic pressure
decreased plasma oncotic pressure
increased capillary permeability
obstructed lymphatic drainage
Question 40
1 / 1 pts
Mr. Fletcher’s CBC indicates which of the following?
pancytopenia
viral infection
iron deficiency
acute leukemia
IncorrectQuestion 41
0 / 1 pts
Mr. Fletcher complains of infectious symptoms related to which of the following?
anemia
thrombocytopenia
Macrocytosis
functional leukopenia
Question 42
1 / 1 pts
Mr. Fletcher's Kaposi Sarcoma involves malignant transformation of which of the following?
connective tissue
glandular tissue
myeloid tissue
epithelial tissue
A CT Scan of the chest reveals a lung mass. The sputum cytology reveals atypical hyperplasia with cells compatible with a diagnosis of Oat cell carcinoma.
Question 43
1 / 1 pts
Oat cell carcinoma of the lung involves malignant transformation of which of the following?
Connective tissue
Epithelial tissue
Pleural tissue
Alveolar macrophages
IncorrectQuestion 44
0 / 1 pts
Considering the organ tropism of lung cancer, which of the following would be closely monitored for?
Increased liver enzymes
Tachycardia
Mental status changes
Pathological fractures
Question 45
1 / 1 pts
Mr Fletcher's electroytes are assessed, including a serum sodium of 128 mg/dl. Mr. Fletcher’s sodium level may be caused by ectopic production of which of the following?
Aldosterone
Calcitonin
ACTH
ADH
The following questions 15 questions refer to the following scenario for Ernestine Lipton
Ernestine Lipton is a 56 year old woman with Systemic Lupus Erythematosus (SLE). She complains of swelling of her hands, face, and feet.
Vital signs are: 37.5C, 78, 26, 164/98
IncorrectQuestion 46
0 / 1 pts
Determination of the cause of the above acid-base imbalance cause can be clarified by evaluation of which of the following?
Albumin
Anion Gap
Glucose
Blood pressure
Question 47
1 / 1 pts
Ms. Lipton has a kidney transplant and is prescribed medications to prevent transplant rejection. Transplant rejection is an example of which of the following?
Type II hypersensitivity reaction
Allergic reaction
Type III hypersensitivity reaction
Alloimmune reaction
Question 48
1 / 1 pts
Ms. Lipton’s electrolyte profile reveals which of the following?
Renal dysfunction and respiratory acidosis
Renal dysfunction and respiratory alkalosis
Renal dysfunction and metabolic acidosis
Renal dysfunction and metabolic alkalosis
Question 49
1 / 1 pts
Ms. Lipton’s ABG reveals which of the following?
MIxed metabolic and respiratory acidosis
Totally compensated respiratory acidosis
Partially compensated respiratory acidosis
Totally compensated metabolic acidosis
IncorrectQuestion 50
0 / 1 pts
Considering the pathophysiology of SLE, Ms. Lipton’s hypertension has likely developed secondary to vasculitis from which of the following?
Cytotoxic T lymphocytes initiating blood vessel damage
Antibodies directed toward the intimal layers of arteries initiating blood vessel damage
Immune complexes becoming deposited in blood vessel walls, initiating inflammatory mediated damage
A normal immune response against beneficial vascular tissue
Question 51
1 / 1 pts
If Ms. Lipton develops Immune Thrombocytopenia Purpura (ITP), the mechanism is which of the following?
Type I hypersensitivity
Type II hypersensitivity
Type III hypersensitivity
Type IV hypersensitivity
IncorrectQuestion 52
0 / 1 pts
Diagnostic criteria for SLE include which of the following?
Stress response
Opportunistic infection
Alloimmunity
Photosensitivity
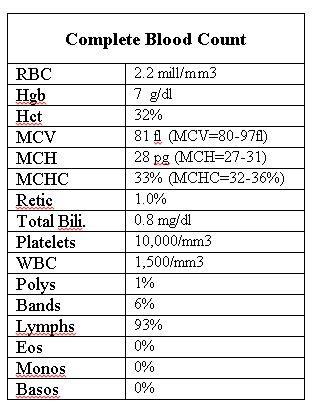
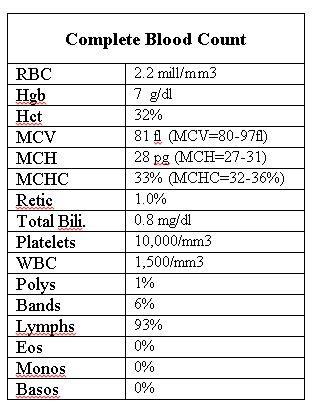
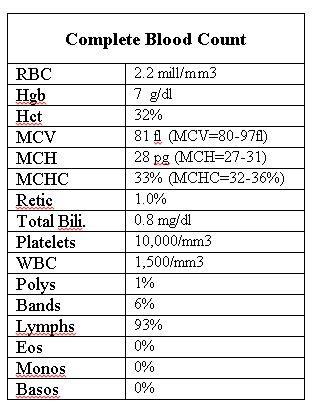
The following Complete Blood Count is assessed:
IncorrectQuestion 53
0 / 1 pts
The above CBC indicates which of the following?
Bacterial infection
Fungal infection
Viral infection
No infection
Question 54
1 / 1 pts
The above CBC indicates which of the following?
Iron deficiency
Folate deficiency
Chronic disease
Hemolysis
Question 55
1 / 1 pts
Ms. Lipton is treated with her prescribed anti-rejection medications. Subsequently her blood counts decrease placing her at risk for developing which of the following?
Acquired Immune Deficiency Syndrome
Opportunistic Infections
Autoimmune diseases
Allergic reactions to medications
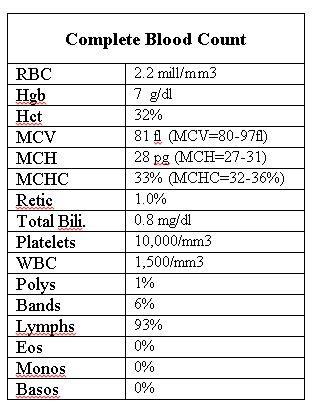
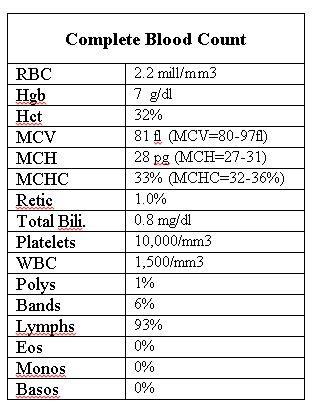
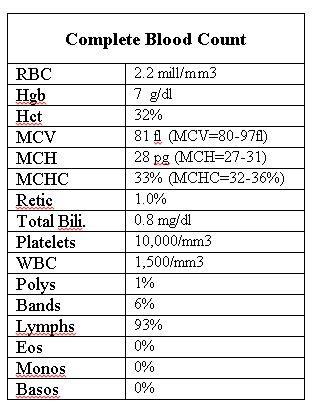
Updated CBC for Ms. Lipton:
Question 56
1 / 1 pts
Ms. Lipton’s CBC indicates which of the following?
a viral infection
immunocompetence
aplastic anemia
tissue hypoxia
IncorrectQuestion 57
0 / 1 pts
Ms. Lipton’s current CBC indicates which of the following?
Iron deficiency
Spontaneous bleeding risk
Chronic infection
Hemolysis
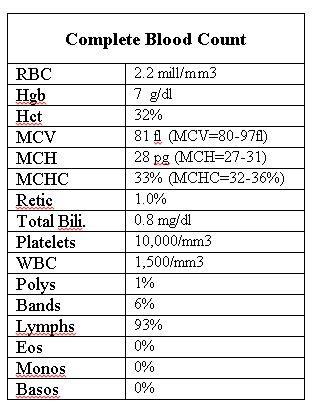
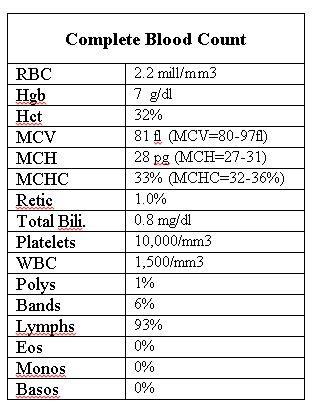
Medications are changed and week later another Complete Blood Count reveals:
IncorrectQuestion 58
0 / 1 pts
Ms. Lipton develops ecchymosis and epistaxis due to which of the following?
Anemia
Thrombocytopenia
Neutropenia
Shift to the right
IncorrectQuestion 59
0 / 1 pts
Ms. Lipton develops fevers related to which of the following?
Anemia
Thrombocytopenia
Neutropenia
Shift to the right
Question 60
1 / 1 pts
Ms. Lipton complains of weakness and dyspnea on exertion associated with which of the following?
Anemia
Thrombocytopenia
Neutropenia
Shift to the right
The following 15 questions refer to the scenario for Gordon Cort
Gordon Cort is a 62 year old man with a new diagnosis of multiple myeloma. Mr.Cort complains of worsening back and leg pain that is intolerable. He has a history of chronic lung disease and complains of developing a cold and a runny nose. He is coughing up thick green mucous with streaks of blood, therefore a specimen is sent to the lab for culture and sensitivity. He is somewhat confused and can’t remember his home address. He is pale, weak, dizzy while walking, with instructions not to get out of bed unless he has assistance.
Vital signs are: 38.9 C, 102, 24, 148/98, 90% sat, pain 8/10.
IncorrectQuestion 61
0 / 1 pts
Mr. Cort’s back and leg pain are likely caused by which of the following?
Thick green mucous with streaks of blood
History of weakness while walking, immobility and now bedrest
Cortical bone destruction and nociceptor stimulation
Chronic anemia, hypoxia, and ischemia
IncorrectQuestion 62
0 / 1 pts
Mr. Cort's mental status most likely been caused by which the following?
his Potassium level
his Magnesium level
his CO2 level
his Calcium level
Question 63
1 / 1 pts
Mr. Cort’s calcium level has most likely been caused by which of the following?
His kidney status and consequent phosphate levels in the blood
Destruction of the cortical bone by mutant cells depositing abnormal IgG
Increased calcitonin production which facilitates calcium absorption
Increased vitamin D production related to his kidney status
Question 64
1 / 1 pts
Mr. Cort’s kidney status has been caused by which of the following?
M Protein deposition
Gram positive cocci
Increased amounts of Immunoglobulin A ( IgA)
Sternberg Reed Cells
Question 65
1 / 1 pts
The above sodium level may be caused by which of the following?
Increased renin
Increased ADH
Increased aldosterone
Increased PTH
Question 66
1 / 1 pts
Mr. Cort's culture and gram stain indicate which of the following?
viruses are present
bacteria are present
fungi are present
no micro-organisms are present
Question 67
1 / 1 pts
Mr. Cort’s activity level places him at risk for developing which of the following?
Increased HDLs
Apnea
Hemoptysis
Thromboemboli
Question 68
1 / 1 pts
Mr. Cort has an increased risk of infection because of which of the following?
Decreased reticulocyte counts
Increased iron levels
Decreased antibody production
Increased calcium levels
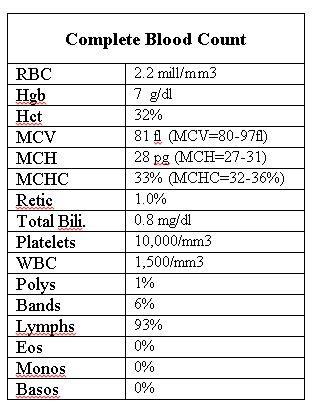
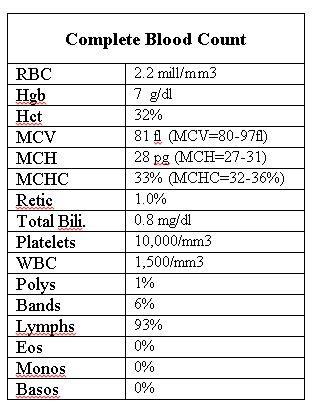
Chemotherapy is administered to Mr. Cort & one week later another CBC reveals:
Question 69
1 / 1 pts
Mr. Cort’s above CBC indicates which of the following?
Immunodeficiency
Bacterial infection
Viral infection
Immunocompetence
Question 70
1 / 1 pts
Mr. Cort develops an elevated uric acid level in his blood, indicating the development of which of the following?
Tumor lysis syndrome
Disseminated intravascular coagulation
alpha 1 antitrypsin deficiency
Pickwickian syndrome
Mr. Cort develops heart failure, with pulmonary edema, hypotension, tachycardia, dyspnea, water retention, and a heart murmur after receiving fluids for his chemotherapy protocol.
Question 71
1 / 1 pts
Which physiologic principle helps explain why receiving fluids can result in heart failure, when a person receives more fluid than their heart can handle?
Pouisseille’s Law
Law of Laplace
Frank-Starling law of the heart
Virchow’s Triad
IncorrectQuestion 72
0 / 1 pts
Mr. Cort has developed jugular venous distension, hepatomegaly and peripheral edema, because of which of the following?
Forward Systolic failure
ACE inhibition
RAA stimulation
Backward Diastolic failure
IncorrectQuestion 73
0 / 1 pts
Mr. Cort’s hypotension and tachycardia are a direct consequence of which of the following?
Backward Diastolic Failure
Increased contractility
Forward Systolic Failure
Right Ventricular Failure
IncorrectQuestion 74
0 / 1 pts
Mr. Cort’s water retention is a consequence of which of the following?
Adrenergic stimulation
RAA stimulation
ACE inhibition
Cholinergic stimulation
Question 75
1 / 1 pts
Mr. Cort’s pulmonary edema is a consequence of which of the following?
Backward Diastolic Failure
Increased contractility
Forward Systolic Failure
Right Ventricular Failure



