Now that you have considered the evidence and potential options to address the local site problem and project objectives, it is now time to describe the proposed design of your project, specific detai
28
Implementation of Type 2 Diabetes Self-Management Education in an Impoverished Community
Leonne M. Reid
NGR 7911
Dr. Valerie Martinez
University of Central Florida
September 26, 2022
(blank placeholder)
Abstract 2
Table of Contents 3
Introduction 5
Background, Significance 5
Description of Organization 7
Mission 8
Organizational Structure 8
Organizational Needs Assessment 8
Organizational Data Indicating a Problem 8
Stakeholder Analysis 10
Patients 10
Professional Organizations 11
Interdisciplinary Colleagues 12
Project Management Tools 13
SWOT Analysis 13
Local Problem Statement 14
Literature Review 15
Description of Search Strategy 15
Inclusion Criteria 15
Search Strategy 16
Quality Appraisal 17
Synthesized Key Findings 17
Interventions Used to Improve the Problem and their Outcomes 17
Peer Support or Coaching or Peer Health Coaching 17
Patient Education 18
Lifestyle Modification Programs 19
Problem-solving or Problem-Solving Therapy 20
Facilitators and Barriers to Implementation of the Interventions Identified 21
Purpose and Project Goals 22
EBP Model 22
References 23
Appendices 29
Appendix A - Summary of Evidence Table 29
Appendix B - Project Management Tools 44
Appendix C - SWOT Analysis 45
Ethnic and racial minority groups in the US, particularly impoverished communities, bear a more significant load from the increasing incidence of Type 2 diabetes (T2D), making the disease a primary focus for disparities in healthcare research (Haw et al., 2021). T2D is a complicated, dire disease in which the weight of self-care is on the patient. In the United States, there are approximately 37.3 million people with diabetes (Centers for Disease Control and Prevention, 2022). Unfortunately, T2D is among the greatest difficult chronic health conditions to manage and control. The increased demand for disease management and the incorporation of complicated self-management routines in the day-to-day lives of diabetics has been proven to lead to increased stress, leaving individuals discouraged, frustrated, and overwhelmed. These demands could also cause depression, anxiety, and reduced well-being (Papelbaum et al., 2010). However, patient behaviors such as lifestyle modifications associated with exercise and diet, medication, record keeping, and daily blood glucose monitoring are crucial in effectively managing the disease (Shrivastava et al., 2013). These behaviors are often referred to as self-management.
Self-management is participating in self-care actions to enhance a person's well-being and behaviors . This considerable burden affects patients from impoverished communities that usually find it challenging to deal with self-management. This is mainly because of cultural, economic, and social barriers, inadequate access to diabetes self-care and self-management resources, and high survival demands among disadvantaged populations (Haw et al., 2021). Recent immigrants and refugees might also experience difficulties adhering to diabetes self-management practices due to various factors, including the absence of preventive care, leading to late treatment and diagnosis (Heerman & Wills, 2011). Cultural differences in how people perceive the origin and treatment of diabetes might also make it challenging to manage the disease among disadvantaged populations (Heerman & Willis, 2011).
Nonetheless, self-management is the most effective way of managing diabetes among populations that lack access to quality healthcare. Most of these practices require considerably less financial resources than frequent healthcare visits. For instance, self-management practices require patients to control and monitor their diet, engage in more physical activity, and monitor their glucose levels, which is more affordable than other management options . However, social support systems might address the effects of environmental and economic challenges that affect effective T2D management by increasing access to social capital, thus promoting self-efficacy behaviors. Nam et al. (2011) state that social support is essential since it is related to the hindrance and facilitation of self-care among patients suffering from chronic diseases like diabetes. Families are the key foundation of social support since they help patients manage their condition successfully.
Ideally, social support is multifaceted and correlates with several social networks (institutional, community-based, occupational, or familial) surrounding a patient (Nam et al. 2011). It has a high potential to exert either negative or positive influences on the person's capability to control the condition independently. A patient's capacity to use social capital to capitalize on established resources could play a significant responsibility in self-care. They could activate constructive social capital resources by seeking and getting help from substantial people in several social positions, such as family members that understand how to manage the disease, thus minimizing the challenges associated with their poverty status that limit them from addressing the condition effectively. In most cases, some attributes of the healthcare system affect effective disease self-care, especially among disadvantaged communities for whom the cost and access to healthcare might provide significant barriers to achieving effective self-management.
Description of OrganizationThe professional organization that is both a stakeholder and a sponsor of this project is the American Diabetes Association (ADA). This organization is committed to printing innovative and timely information and publishing research for professionals specializing in diabetes care, treatment, research, and education (ADA, 2022). It is a non-profit membership organization that promotes the efforts of healthcare professionals to cure and prevent diabetes by enhancing the well-being of people with diabetes (ADA, 2022). ADA offers research grant awards, patient information programs or materials, and professional education programs and helps spread public awareness of diabetes. The organization's technology assessment activities are publishing review articles, creating position papers, and sponsoring and funding consensus conferences. ADA also sponsors conferences, research symposia, and annual postgraduate courses that intend to spread new diabetes information or discuss crucial topics related to the disease.
Mission"To offer the public and healthcare professionals comprehensive and correct information on technologies (drugs, medical devices, surgical or medical procedures among others) that are relevant to diabetes" (ADA, 2022).
Organizational StructureThe board members, professional members, and officers of the American Diabetes Association (ADA) often request for research to be conducted. Formal written requests are then submitted to the senior staff or volunteer leadership, who then set the research topic priorities. Research is often performed by assessors or researchers that have expertise in areas related to diabetes, such as public health, law, nutrition, medicine, and exercise. The key methods used in the assessments include cost analyses, group judgment, expert opinion, and information synthesis (Council on Health Care Technology, 2008).
Organizational Needs Assessment Organizational Data Indicating a ProblemAccording to the National Diabetes Statistics Report, roughly 8.2% of the United States population (26.9 million individuals) were diagnosed with diabetes in 2018 (Center for Disease Control and Prevention, 2020). In 2016, around 12.6 % of US citizens in non-metropolitan regions were diagnosed with diabetes, a higher statistic than 9.9 % in metropolitan regions (Center for Disease Control and Prevention, 2020). In the 'diabetes belt', the incidence of diabetes was about 11.7 % of the entire US population. Over one-third of counties within the diabetic belt are located in the Appalachian Region. Many states within the belt are extremely rural compared to the United States average (Centers for Disease Control and Prevention, 2022). These statistics show that diabetes is a major concern within impoverished and rural communities because of limited access to healthcare services and a higher prevalence of risk factors (Misra et al., 2019). For instance, impoverished communities often comprise populations at a higher risk of T2D, such as ethnic and racial groups and older adults (Mendenhall et al., 2017).
Additionally, several barriers affect patient education and quality healthcare access in impoverished communities. First, fewer transport options in rural areas make it challenging for T2D patients to travel to doctor appointments (Stotz et al., 2021). Secondly, there are higher rates of uninsured patients in rural communities. Limited access to medical covers makes it difficult for impoverished populations to access medical supplies, medications, and cover medical appointments. Also, there are fewer healthcare providers in poor communities, making it difficult to offer patient education, replace retiring healthcare professionals, and retain nutritionists and dietitians. Workforce shortages in impoverished societies also limit access to specialized healthcare professionals, including endocrinologists (North et al., 2022).
These data indicate a major problem within impoverished communities since T2D patients would fail to access pharmacological interventions for managing the disease. However, with the introduction of self-management practices, individuals in rural communities could learn about some of the efficient lifestyle modifications they should make to control their weight and glycemic levels. Self-management is cheaper and less cumbersome because it only requires the efforts of a patient and their family to manage the disease .
Stakeholder AnalysisThe main stakeholders relevant to this research include patients, their families, the family advisory committee, professional organizations such as the American Diabetes Association (ADA), and interdisciplinary colleagues such as respiratory therapists, nutritionists, physicians, or occupational therapists (OT)/PT.
PatientsPatients are the main stakeholders in this project because the project will have a significant impact on them. This project will help patients understand how self-care and self-management could help manage T2D. Their families will also benefit from the project because they will be able to recognize effective strategies to incorporate self-management into their management regimen. Another major thing that patients, family advisory committees, and relatives need to understand from the project is examples of self-management interventions that have been proven effective in managing T2D. Patients and their families are also a great asset to the project because they will contribute by taking part in the project and having outcomes measured like HbA1c and glycemic levels, weight, and quality of life . Also, families of patients with the disease can contribute to the project by providing crucial information on the efficacy of the self-management interventions they have used on their relatives. However, patients might impede the project by providing false information on self-management efficiency and failing to commit to self-management interventions. Families can also affect the project by failing to give their relatives with type II diabetes the correct self-management interventions during the study period. The engagement of patients and their families in this project requires that self-care and self-management education be offered.
Professional OrganizationsUtilizing professional organizations such as the American Diabetes Association (ADA) will help inform the project and have them approve whether the identified strategies are safe and effective in managing T2D. These organizations would contribute to the project by offering the study's respondents patient education . They could also fund the research since the American Diabetes Association (ADA) often funds studies to control, treat, and prevent diabetes (ADA, 2022). The main way that professional organizations could impede the project is by refusing to fund and contribute to the project . The best way to engage professional organizations is having them offer patient education on safe self-management practices for T2D.
Interdisciplinary ColleaguesIn a healthcare setting, an interdisciplinary team consists of practitioners from different disciplines that work together to address a patient's psychological and physical needs ( Indeed, 2021 ). For instance, for a patient with T2D, the interdisciplinary team comprises respiratory therapists, nutritionists, occupational therapists, and other physicians. These stakeholders are crucial to the project because they will help inform the project and approve the self-management practices recommended at the end of the project. The main thing that this group of stakeholders is concerned with is whether self-management interventions are effective in managing T2D. This project will help them understand which patient education they need to provide to these patients and the self-management practices they would recommend to patients other than pharmacological interventions. Interdisciplinary colleagues could also contribute significantly to the project. For instance, nutritionists are well-equipped with the correct information on healthy diets for patients suffering from different diseases. Therefore, in this project, they will help recommend healthy lifestyles and dietary changes which would help control HbA1c and glycemic levels and weight. Additionally, occupational therapists (OT) are healthcare professionals that help injured, disabled, or sick patients improve, recover, or develop by maintaining the life skills needed for healthy living (Burson, Fette, & Kannenberg, 2017). Therefore, they could help T2D patients maintain, recover, and develop meaningful occupations or activities for communities, groups, and individuals.
The interdisciplinary team could affect or obstruct this project when they do not recommend and administer appropriate and efficient self-management interventions for the project participants . For instance, if a nutritionist recommends a diet that would not be effective in reducing glycemic levels in a patient with T2D, then the project findings will be a ffected . Similarly, suppose an occupational therapist does not help a patient to develop a healthy lifestyle to manage the disease adequately. Patient health outcomes will be affected in that case, impacting the project's findings.
Project Management Tools SWOT AnalysisSeveral factors would impede the efficient implementation of this study in the given practice setting (See Appendix C for the SWOT Analysis diagram of these factors).
Strengths
i. There is access to respondents who would help provide information on which strategies they have adopted and utilized in the effective management of T2D other than pharmaceutical interventions since the given setting is impoverished communities .
ii. There is the availability of experienced researchers and professionals (such as nutritionists and occupational therapists) to help recommend effective self-management interventions to the study 's respondents.
Weaknesses
i. Lack of funding because there are fewer financial resources in impoverished communities; hence project initiators must fund the project themselves or look for a professional organization willing to fund the research.
ii. Limiting beliefs among individuals , such as using cultural interventions like traditional herbs and ayurvedic medications, is the most effective way of preventing and treating T2D (Ahmad, 2021). These beliefs might impede the effective implementation of self-management interventions.
Opportunities
i. Increased interest among professional organizations and leading scientific institutions to research effective disease management strategies. For example, the American Diabetes Association has emerged to help fund research on effective T2D management, provide education on self-management practices that would help manage the disease and recommend healthy diets for the patients (ADA, 2022).
ii. The availability of professional organizations which help provide education to patients with T2D in impoverished communities.
Threats
i. Language and cultural barriers. Researcher s might find it difficult to communicate with T2D patients from impoverished communities.
Local Problem StatementT2D patients in impoverished communities have limited access to healthcare services due to different factors, such as geographical and financial barriers; this accounts for the high rates of T2D within these communities since patients lack professionals to guide them through pharmacological interventions. These high statistics could be mitigated through dietary and lifestyle modifications. Because treatments such as insulin and drugs are expensive and impoverished communities have fewer resources, it is important to prioritize prevention and manage the disease using self-management practices. It is also essential to spread awareness and educate patients on how lifestyle changes could be as effective as using drugs to manage and prevent T2D.
Literature Review Description of Search Strategy Inclusion CriteriaI screened this topic independently and then selected articles for quality appraisal and inclusion criteria. Once the pieces were screened, I developed a quality appraisal and inclusion criteria. For the articles to be included in the official review, they were analyzed using the following inclusion criteria. The article must have the following:
i. Provided quantitative and qualitative empirical (descriptive, cohort study, quasi-experimental, RCT, systematic review, or meta-analysis) evaluative support.
ii. Identified an intervention.
iii. Included an outcome variable of self-care and self-management.
iv. Included adult respondents with type II diabetes.
v. Operationalized as a psychosocial indicator (such as support, stage of change, depression, stress, or emotional adjustment), physiological indicator (such as cholesterol, HbA1c, weight, blood pressure, blood glucose level), self-management outcomes (such as SBGM pattern, medication, exercise, diet) and knowledge.
Search StrategyAn all-inclusive search was performed through Ebscohost utilizing the following databases: PsycInfo, PsycArtiCLES, MEDLINE, Health Source: Nursing/Academic Edition, CINAHL, and Academic Search Complete. The search was conducted to establish best practices in self-management interventions for T2D. The top search terms used include randomized controlled trials, self-management, patient education, self-care, type 2 diabetes, and diabetes mellitus. Only peer-reviewed articles written in English between January 2015 to 2022 were selected. Additionally, the Cochrane Library was looked up for self-management review. The first search yielded 62 peer-reviewed articles abstracted for self-management intervention topics. Forty -six articles were excluded since they failed to meet the inclusion criteria because they focused on T1D rather than T2D. Duplicates were removed from search results. The themes of the remaining sixteen articles selected for review included patient education, lifestyle modification programs, peer support, and lifestyle adaptation. The reference lists of the selected articles were then analyzed to locate other relevant articles in the search. At the end of the reviews and search, 14 articles were chosen for synthesis. All articles chosen for review were critically appraised using the Johns Hopkins Evidence-Based Practice Model Heirchy of Evidence guide. The quality of the articles selected for this review could be summarized as high-quality randomized clinical trials (n=1), good-quality systematic reviews (n=2), good-quality meta-analysis (n=1), low-quality integrative review (n=1), high-quality qualitative descriptive study (n=11), and good quality literature reviews (n=4). See Appendix H for evidence table.
Synthesized Key Findings Interventions Used to Improve the Problem and their Outcomes Peer Support or Coaching or Peer Health CoachingPeer support, peer coaching, and health coaching utilize volunteers or health care providers, often referred to as peer supporters or coaches, to offer self-management care to individuals with the same healthcare condition as them or those they consider their peers (Thom et al., 2013; Ghorob et al., 2011). These peers and coaches could include healthcare professionals, family members, educators, community health workers, and patients. Ideally, peer health coaching is done to connect a patient to other patients that have the same health issues. Regardless of peer support or coaching, the objective is to motivate and engage T2D patients in self-care and self-management. Peer support and coaching interventions have been adequately researched in disease education. Tang et al. (2011) explain that in diabetes self-management, peers and coaches play multiple roles, such as group facilitator, mentor, case manager, educator, cultural translator, and advocate. Peer support and coaching are often delivered by trained professionals and primarily emphasize self-management interventions based on documented curricula and time-limited. Based on efficiency, support and peer health coaching have effectively helped lower HbA1c levels and improve self-management (Powers et al., 2015; Moskowitz et al., 2013). Due to such favorable results, peer support and health coaching have received significant interest as effective interventions for disease self-care (Aschbrenner et al., 2015).
Patient EducationDiabetes self-management education (DSME) has been the most common and effective strategy for managing diabetes (Pamungkas, Chamroonsawasdi, & Vatanasomboon, 2017). This intervention program has evolved over the decades to include biopsychosocial treatment models and affective and behavioral tactics to deal with the psychosocial and medical requirements of individuals with T2D (Carpenter, DiChiacchio, & Barker, 2019). Patient education could be administered in different modalities, to groups or individuals, professionals or peers, in extended or short-term sessions. DSME entails various crucial components that should be maintained to prevent complications related to diabetes- monitoring checks, physical activity, adherence to diet, and treatments (Carpenter, DiChiacchio, & Barker, 2019). Powers et al. (2015) found that implementing self-management education effectively improves the quality of life for T2D .
Lifestyle Modification ProgramsLifestyle modification programs are used to improve health outcomes through behavior and lifestyle changes. Lifestyle modification programs could comprise a variety of topics such as stress management, exercise, diet, and medications (Carpenter, DiChiacchio, & Barker, 2019). Lifestyle modification programs have had a long history in managing diabetes because it usually combines interventions targeting behavior modification, exercise, diet, and medication management. Lifestyle modification programs such as self-efficacy, healthy diets, and greater exercise have helped patients with T2D manage their weight and control their glycemic and HbA1c levels (Delahanty et al., 2013; Kerrison et al., 2017; Carpenter, DiChiacchio, & Barker, 2019).
Problem-solving or Problem-Solving TherapyProblem-solving therapy (PST) is a strategy for behavioral modification used to determine what needs to be done to attain a goal that is not apparent (Carpenter, DiChiacchio, & Barker, 2019). Problem-solving therapy aims to minimize adverse emotional reactions, change behavior, and improve positive emotional responses (Zhang et al., 2018). Problem-solving therapy entails teaching individuals suffering from a chronic disease how to deal with life issues by breaking them down into two different sections: utilizing problem-solving skills and employing problem-solving orientations to life. Additionally, problem-solving therapy mainly focuses on teaching a patient skills such as recognizing the health issue, defining the problems, comprehending them, setting health objectives associated with the health issue, identifying alternative strategies to solve the health issue, analyzing and selecting the best methods, implementing these alternatives, and analyzing their effort in solving the problem (Nezu et al., 2012).
Problem-solving therapy (PST) has had an extended history in counseling and clinical mindset to deal with substance abuse, coping skills and stress management, relational and family distress, and several mental health disorders. Additionally, problem-solving therapy has been constantly used within diabetes care and education and is recognized as a crucial skill, intervention, and process in diabetes self-management (Carpenter, DiChiacchio, & Barker, 2019).
Facilitators and Barriers to Implementation of the Interventions IdentifiedBarriers to T2D self-management include lack of support, shortage of resources, inadequate behavioral beliefs and knowledge, and suffering from health issues (Shi et al., 2020). When patients lack support from their families (such as lack of emotional support, taking medications, and eating healthy) and professionals, it interferes with the efficacy of self-management interventions. Some health issues, such as insomnia, physical discomfort, and hyperglycemia, could also interfere with self-care (Shi et al., 2020). These issues reduce patient motivation to engage in self-management interventions. Moreover, the shortage of resources, such as limited access to patient education, lack of finances to buy healthy foods, little blood glucose monitoring, and unavailability of hypoglycemic medications.
Lastly, inadequate behavioral beliefs, knowledge, and confusion about taking diabetes medications interfere with the efficacy of diabetes self-management (Kulhawy-Wibe et al., 2018). Shi et al. (2020) found that many diabetic patients did not understand how to use hypoglycemic agents. Many were confused about the medications' side effects, usage, and names, which prevented them from efficiently managing diabetes. Recognizing these barriers is essential in creating effective strategies, including promoting successful self-management, implementing patient-centered care, reinforcing social and medical support, and creating favorable environments. Also, understanding these barriers will help patients understand how they will deal with them and educate their families and peers on how they can help them manage the disease on their own.
Purpose and Project GoalsThe project aims to answer the EBP question of whether self-management effectively manages T2D in impoverished communities . Self-management could be one of the best alternatives for managing T2D among communities with inadequate access to quality healthcare since fewer financial resources are required than pharmacological means (Whittemore et al. 2019). For example, because T2D is mainly developed from poor diet and lifestyle practices, modifications such as eating a cleaner diet, exercising more often, and tracking glucose levels could help manage the disease. However, factors such as limiting beliefs among rural residents and lack of support from family could impede the effective use of self-management to control T2D (Shi et al. 2020). Therefore, this research will examine how such barriers could be addressed to ensure that patients manage T2D effectively without experiencing dire health effects. It will also look at how patient education could be improved within impoverished communities so that people with diabetes could learn how to manage the disease independently without the intervention of healthcare professionals.
EBP ModelThis project utilizes the Johns Hopkins Nursing Evidence-Based Practice Model (JHNEBP). This model is structured to satisfy EBP needs by employing a simple process known as Practice Question, Evidence, and Translation(PET; Christenberry , 2017). In the first step, the EBP question is created, followed by searching, appraising, describing, and rating the quality of evidence. In the last step, feasibility of the project is determined, an action plan for implementation is created, and evidence-based practice changes are implemented (Christenberry, 2017). Also, findings are presented to the larger nursing faculty and healthcare organizations.
Ahmad, A. (2021). Medication-taking behavior and treatment preferences of Indian migrants with type 2 diabetes in Australia (Doctoral dissertation).
American Diabetes Association (2022). About Us. https://diabetes.org/about-us
Aschbrenner, K. A., Naslund, J. A., Barre, L. K., Mueser, K. T., Kinney, A., & Bartels, S. J. (2015). Peer health coaching for overweight and obese individuals with serious mental illness: intervention development and initial feasibility study. Translational Behavioral Medicine, 5(3), 277-284.
Burson, K., Fette, C., & Kannenberg, K. (2017). Mental health promotion, prevention, and intervention in occupational therapy practice. AJOT: American Journal of Occupational Therapy, 71(S2), 7112410035p1-7112410035p1.
Carpenter, R., DiChiacchio, T., & Barker, K. (2019). Interventions for self-management of type 2 diabetes: an integrative review. International Journal of Nursing Sciences, 6(1), 70-91.
Center for Disease Control and Prevention (2022). Appalachian Diabetes Control and Translation Project. https://www.cdc.gov/diabetes/health-equity/appalachian.html
Christenbery, T. L. (2017). Evidence-based practice in nursing: Foundations, skills, and roles. Springer Publishing Company.
Center for Disease Control and Prevention (2020). National Diabetes Statistics Report 2020. Estimates of Diabetes and Its Burden in the United States. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
Council on Health Care Technology. (2008). Medical Technology Assessment Directory: A Pilot Reference to Organizations, Assessments, and Information Resources. National Academies Press.
Delahanty, L. M., Peyrot, M., Shrader, P. J., Williamson, D. A., Meigs, J. B., Nathan, D. M., & DPP Research Group. (2013). Pretreatment, psychological, and behavioral predictors of weight outcomes among lifestyle intervention participants in the Diabetes Prevention Program (DPP). Diabetes Care, 36(1), 34-40.
Ghorob, A., Vivas, M. M., De Vore, D., Ngo, V., Bodenheimer, T., Chen, E., & Thom, D. H. (2011). The effectiveness of peer health coaching in improving glycemic control among low-income patients with diabetes: protocol for a randomized controlled trial. BMC Public Health, 11(1), 1-6.
Heerman, W. J., & Wills, M. J. (2011). Adapting models of chronic care to provide effective diabetes care for refugees. Clinical Diabetes, 29(3), 90-95.
Indeed (2021). What Is an Interdisciplinary Team? Definition, Importance, and Advantages. https://www.indeed.com/career-advice/finding-a-job/interdisciplinary-team
Mendenhall, E., Kohrt, B. A., Norris, S. A., Ndetei, D., & Prabhakaran, D. (2017). Non-communicable disease syndemics: poverty, depression, and diabetes among low-income populations. The Lancet, 389(10072), 951-963.
Misra, A., Gopalan, H., Jayawardena, R., Hills, A. P., Soares, M., Reza‐Albarrán, A. A., &
Ramaiya, K. L. (2019). Diabetes in developing countries. Journal of Diabetes, 11(7),
522-539
Moskowitz, D., Thom, D. H., Hessler, D., Ghorob, A., & Bodenheimer, T. (2013). Peer coaching to improve diabetes self-management: which patients benefit most? Journal of General Internal Medicine, 28(7), 938-942.
Nam, S., Chesla, C., Stotts, N. A., Kroon, L., & Janson, S. L. (2011). Barriers to diabetes management: patient and provider factors. Diabetes Research and Clinical Practice, 93(1), 1-9.
Nezu, A. M., Nezu, C. M., & D'Zurilla, T. (2012). Problem-solving therapy: A treatment manual. Springer Publishing Company.
North, S., Crofts, C., & Zinn, C. (2022). Health professionals' views and experiences around the dietary and lifestyle management of gestational diabetes in New Zealand. Nutrition & Dietetics, 79(2), 255-264.
Kerrison, G., Gillis, R. B., Jiwani, S. I., Alzahrani, Q., Kok, S., Harding, S. E., ... & Adams, G. G. (2017). The effectiveness of lifestyle adaptation for the prevention of prediabetes in adults: a systematic review. Journal of Diabetes Research, 2017.
Kulhawy-Wibe, S., King-Shier, K. M., Barnabe, C., Manns, B. J., Hemmelgarn, B. R., & Campbell, D. J. (2018). Exploring structural barriers to diabetes self-management in Alberta First Nations communities. Diabetology & Metabolic Syndrome, 10(1), 1-7.
Pamungkas, R. A., Chamroonsawasdi, K., & Vatanasomboon, P. (2017). A systematic review: family support integrated with diabetes self-management among uncontrolled type II diabetes mellitus patients. Behavioral Sciences, 7(3), 62.
Papelbaum, M., Lemos, H. M., Duchesne, M., Kupfer, R., Moreira, R. O., & Coutinho, W. F. (2010). The association between quality of life, depressive symptoms and glycemic control in a group of type 2 diabetes patients. Diabetes Research and Clinical Practice, 89(3), 227-230.
Powers, M. A., Bardsley, J., Cypress, M., Duker, P., Funnell, M. M., Hess Fischl, A., ... & Vivian, E. (2015). Diabetes self-management education and support in type 2 diabetes: A joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabetes Care, 38(7), 1372-1382.
Shi, C., Zhu, H., Liu, J., Zhou, J., & Tang, W. (2020). Barriers to self-management of type 2 diabetes during COVID-19 medical isolation: a qualitative study. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy, 13, 3713.
Shrivastava, S. R., Shrivastava, P. S., & Ramasamy, J. (2013). Role of self-care in management of diabetes mellitus. Journal of diabetes & Metabolic Disorders, 12(1), 1-5.
Stotz, S. A., Ricks, K. A., Eisenstat, S. A., Wexler, D. J., & Berkowitz, S. A. (2021). Opportunities for Interventions That Address Socioeconomic Barriers to Type 2 Diabetes Management: Patient Perspectives. The Science of Diabetes Self Management and Care, 47(2), 153-163.
Tang, T. S., Funnell, M. M., Gillard, M., Nwankwo, R., & Heisler, M. (2011). Training peers to provide ongoing diabetes self-management support (DSMS): results from a pilot study. Patient Education and Counseling, 85(2), 160-168.
Thom, D. H., Ghorob, A., Hessler, D., De Vore, D., Chen, E., & Bodenheimer, T. A. (2013). Impact of peer health coaching on glycemic control in low-income patients with diabetes: a randomized controlled trial. The Annals of Family Medicine, 11(2), 137-144.
Whittemore, R., Vilar-Compte, M., De La Cerda, S., Marron, D., Conover, R., Delvy, R., ... & Pérez-Escamilla, R. (2019). Challenges to diabetes self-management for adults with type 2 diabetes in low-resource settings in Mexico City: a qualitative descriptive study. International Journal for Equity in Health, 18(1), 1-10.
Zhang, A., Park, S., Sullivan, J. E., & Jing, S. (2018). The effectiveness of problem-solving therapy for primary care patients' depressive and/or anxiety disorders: A systematic review and meta-analysis. The Journal of the American Board of Family Medicine, 31(1), 139-150.
Appendices Appendix A - Summary of Evidence Table| EBP Question: For type II diabetics in impoverished communities, is the implementation of self-management effective? | ||||||||||
| Author and Date | Title of Article | Population, size (n) | Setting | Type of Evidence | Description of Intervention | Outcome Measures | Findings that Help Answer the EBP Question | Limitations | Evidence Level and Quality | Implications for Proposed Project |
| Authors: Margaret A. Powers, Joan Bardsley, Marjorie Cypress, Paulina Duker, Martha M. Funnell, Amy Hess Fischl, Melinda D. Maryniuk, Linda Siminerio, & Eva Vivian Publication Date: 5 June 2015 | Diabetes Self-management Education and Support in Type 2 Diabetes: A Joint Position Statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics | N/A | N/A | Literature Review | This is a study of a given phenomenon through a thorough survey of peer-reviewed articles. | Quality of life. | Type II diabetes is a burdensome and complex disease that demands individuals to make rational health decisions to maintain a healthy lifestyle. The implementation of self-management is therefore effective for diabetics in rural communities where they would have difficulty accessing healthcare resources. | This literature review did not incorporate a section highlighting the limitation. Nonetheless, there are minor differences between the findings of these articles. | The findings of this article are consistent and hence adequate to be used in the project. | This article will help build on the research concerning the importance of introducing self-management care for diabetes type II in impoverished communities. |
| Authors: Morgan Griesemer Lepard, Alessandra L. Joseph, April A. Agne & Andrea L. Cherrington Publication Date: 7 May 2015 | Diabetes Self-Management Interventions for Adults with Type 2 Diabetes Living in Rural Areas: A Systematic Literature Review | N/A | N/A | Literature Review | This is a study of a given phenomenon through a thorough survey of peer-reviewed articles. | Rates of type II diabetes | The authors found that in impoverished communities, there are higher rates of type II diabetes due to limited access to diabetes education, health services, and community resources. However, interventions such as collaborative goal-setting and motivational support are likely to enhance the metabolic control of a diabetic. | Possible publication bias. Difficulty comparing data from several articles. The interventions analyzed were of different lengths and designed for several cultural groups hence making it difficult to compare the studies. | The evidence provided by this article is sufficient, however, the inconsistencies in the results in different articles interfere with the validity of the results. | The findings from this article will be used to build on the research since the results indicate that there is a positive impact of self-management care for diabetics in rural communities. |
| Authors: Roger Carpenter, Toni DiChiacchio & Kendra Barkera Publication Date: 10 Jan 2019 | Interventions for self-management of type 2 diabetes: An integrative review | N/A | N/A | Integrative review | It is a methodology that summarizes past theoretical and empirical literature to offer a comprehensive comprehension of a phenomenon. | HbA1c level. | A significant amount of literature showed that self-management has a short-term improvement in distress reduction and glycemic control. | Due to the exhaustive nature of the existing evidence on this phenomenon, it is difficult to be informed about the entire body of literature on this topic. | The evidence offered by this article is inadequate because different articles reveal different results on the efficacy of self-management in diabetes care. | Implications remain inconclusive. |
| Authors: Fadli, F. Publication Date: 2022 | The Impact of Self-Management-Based Care Interventions on Quality of Life in Type 2 Diabetes Mellitus Patients: A Philosophical Perspective | N/A | N/A | Literature Review | This is a study of a given phenomenon through a thorough survey of peer-reviewed articles. | The quality of life of type 2 diabetes mellitus patients. | Most articles indicated an increase in the quality of life and self-care behaviors among type 2 diabetes patients after being subjected to self-management interventions. | Some articles did not indicate a major difference in the quality of life among diabetics utilizing self-management in impoverished communities. | The article provides valid evidence because most of the articles reviewed provided similar results. | Since this article indicates a positive relationship between self-management and diabetics in impoverished societies, it will be used to build research on the topic. |
| Authors: Burd, C., Gruss, S., Albright, A., Schumacher, P. & Alley, D. Publication Date: 28 Jan 2022 | Translating knowledge into action to prevent type 2 diabetes: Medicare expansion of the National Diabetes Prevention Program lifestyle intervention. | Over 3,000 adults | RCT groups | Literature Review | This is a study of a given phenomenon through a thorough survey of peer-reviewed articles. | Rate of Diabetes Type II among groups using medicine and self-management. | The self-management group indicated a 71% rate of reducing the effects of diabetes type II while the group using metformin indicated a 31% likelihood of managing the disease. | Racial inequality because a majority of the respondents were not at a high risk of developing diabetes type 2. | High-quality evidence because there are expert opinions from Medicaid Innovation Center. | Results will help answer the EBP question and build on the research. |
| Authors: Yamaoka, K., Nemoto, A., & Tango, T. Publication Date: 19 June 2019 | Comparison of the Effectiveness of Lifestyle Modification with Other Treatments on the Incidence of Type 2 Diabetes in People at High Risk: A Network Meta-Analysis | n=113 | Online research PUBMED database | Meta- analysis | An epidemiological, formal, and quantitative study design is utilized to systematically analyze the findings of past research on a given topic. | Quality of life of diabetics. | Findings indicate that self-management through lifestyle modifications help prevent the progression of type 2 diabetes. | The type of education training utilized was ununiform among different studies. The study only used PUBMED in the review. | Good quality of evidence because the sample used was adequate. However, some articles provide inconsistent results. | The findings will be used to supplement the findings of other articles on the same topic. |
| Authors: Kerrison, G., Gillis, R. B., Jiwani, S. I., Alzahrani, Q., Kok, S., Harding, S. E., Shaw, I. & Adams, G. G. Publication Date: 16 Apr 2017 | The Effectiveness of Lifestyle Adaptation for the Prevention of Prediabetes in Adults: A Systematic Review | Population: 1,780 studies n:9 studies | Electronic Databases such as CENTRAL, Cochrane, PsycINFO, EMBASE, MEDLINE, CINAHL | Systematic Review | Summary of literature that use reproducible and explicit methods to synthesize, critically appraise, and search a particular issue. | Glycemic control, weight changes, BMI, and physical exercise capacity. | Self-management such as changing lifestyle behaviors helps minimize the incidence of diabetes type 2. | Minor differences in the findings of the studies. | High-quality evidence | These results will help formulate the final project's report on the efficacy of self-management in individuals with diabetes type II. |
| Authors: Walker, R. J., Strom Williams, J., & Egede, L. E. Publication Date: April 2016 | Influence of Race, Ethnicity, and Social Determinants of Health on Diabetes Outcomes | N/A | N/A | Systematic Review | Summary of literature that use reproducible and explicit methods to synthesize, critically appraise, and search a particular issue. | Quality of life | Even though the findings of this article do not address the evidence-based question directly, it helps highlight factors that might affect certain groups from receiving treatment such as economic classes. | Limited evidence on how ethnicity and race affect the quality of health outcomes of diabetics in impoverished communities. | The evidence provided is of moderate quality. | The findings of this article could be used to explain some of the factors that prevent diabetics in impoverished communities from accessing medical care services. This will help indicate a need for the implementation of self-management. |
| Authors: Delahanty, L. M., Peyrot, M., Shrader, P. J., Williamson, D. A., Meigs, J. B., Nathan, D. M., & DPP Research Group. Publication Date: 2013 | Pretreatment, Psychological, and Behavioral Predictors of Weight Outcomes Among Lifestyle Intervention Participants in the Diabetes Prevention Program (DPP) | n: 274 | DPP community centers | Randomized clinical trial | Assigning respondents to different groups (control group and treatment group) that receive different treatments. | Weight loss. | Self-efficacy, healthy diets, and greater exercise helped 40.5% of the participants in the Diabetes Prevention Program (DPP) achieve their weight loss goal. | The participants in this study did not fully represent all diabetics trying to lose weight. | The evidence provided is high quality. | These findings show that self-management could help diabetes manage the disease. |
| Authors: Whittemore, R., Vilar-Compte, M., De La Cerda, S., Marron, D., Conover, R., Delvy, R., & Pérez-Escamilla, R. Publication Date: 23 August 2019 | Challenges to diabetes self-management for adults with type 2 diabetes in low-resource settings in Mexico City: a qualitative descriptive study | n: 20 adults | 3 Seguro Popular primary care clinics in Mexico City | Qualitative descriptive study | This approach systematically describes a phenomenon. | Glycemic targets. | Factors that interfere with the efficacy of self-management in diabetics include lack of resources, mental health issues, cultural beliefs, and lack of family support. | The sample was in a single geographical location hence it does not mirror the situation in other impoverished regions. | High-quality evidence. | The findings could be used in the project to show how self-management helps patients in impoverished societies manage the disease. |
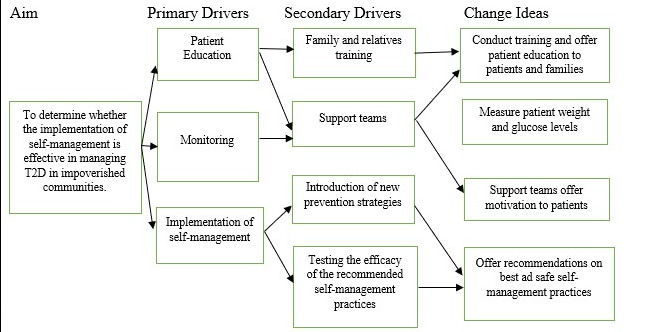
Figure 1: Driver Diagram
| Strengths
| Weaknesses
|
| Opportunities
| Threats
|
Table 2: SWOT Analysis



