In this unit you will compose and submit an informative abstract along with the other pieces of your paper which you have been working on in Units II through VI. Within your research paper template, p
Effects of Alzheimer’s Disease on Cognitive and Behavioral Functions 21
The Effects of Alzheimer's Disease on Cognitive and Behavioral Functions
Name
University
The Effects of Alzheimer's Disease
Alzheimer's disease (AD) is an irreversible and progressive brain disorder affecting millions worldwide. AD is the most typical dementia cause in older adults, accountable for up to 70% of all cases (Scheltens et al., 2021). AD is categorized by the accumulation of abnormal proteins, like amyloid-beta and tau, in the brain, which leads to the degeneration and death of brain cells, particularly in areas involved in memory, learning, and reasoning. AD is a major public health issue that has significant social and economic consequences, as it affects not only the individuals with the disease but also their families and caregivers and places a substantial burden on healthcare systems and society as a whole.
Hypothesis. The main hypothesis of this paper is that AD has a profound impact on cognitive and behavioral functions leading to significant impairment in daily activities, social interactions, and quality of life that eventually led to needing assistance and/or a caregiver. This hypothesis will be supported by a review of the literature on the clinical manifestations and neuropsychological deficits associated with AD.
Key Terms
Alzheimer’s disease: This is a disorder (neurodegenerative) that influences cognitive and behavioral functions and is characterized by the accumulation of abnormal proteins in the brain (Peña-Casanova et al., 2021).
Dementia: a broad term that refers to a decline in cognitive function, including memory, language, and reasoning, that interferes with daily activities (Warren, 2022).
Neuropsychological deficits: impairments in cognitive functions, like attention, language, memory, and executive functions, that are associated with neurological conditions (Peña-Casanova et al., 2021).
Amyloid-beta: a protein that forms plaques in the brains of individuals with AD (Peña-Casanova et al., 2021)
Tau: a protein that forms tangles in the brains of individuals with AD (Peña-Casanova et al., 2021).
Treatment for AD. Current research indicates that natural compounds may have therapeutic promise for Alzheimer's disease (AD). It has been discovered that numerous natural products contain phenolics, terpenoids, alkaloids, glycosides, and vitamins, which contribute to their medicinal benefits. In a recent study, Rahman, Islam, and Emran (2022) highlighted numerous clinically significant natural products for their potential to treat AD. The writers began by discussing the anti-protective Alzheimer's benefits of green tea. They noted that drinking green tea daily is connected with a reduced risk of AD and its progression. In addition, they discussed the effects of berberine, an alkaloid isolated from the root and stem of Berberis plants that have been demonstrated to have substantial anti-AD properties. The researchers highlighted the anti-inflammatory, antioxidant, and neuroprotective properties of curcumin, a polyphenol present in turmeric.
Benefits of Fatty Acids. The authors also examined the possible advantages of omega-3 fatty acids, which have been found to lower the risk of Alzheimer's disease and enhance cognitive function. They discussed the neuroprotective, anti-inflammatory, and antioxidant properties of resveratrol, a polyphenol found in grapes and other foods. Animal models have demonstrated that pomegranate extract has benefits on cognitive function. The authors concluded that natural compounds might be potential alternatives to conventional treatments for Alzheimer's disease. This review emphasized the therapeutic potential of various natural compounds for Alzheimer's disease and encouraged additional investigation into their efficacy. It was discussed the preventive properties of resveratrol, a polyphenol found in grapes and other fruits showing anti-inflammatory, antioxidant, and neuroprotective properties. They explored the potential of pomegranate extract, which has been shown to benefit cognitive performance in animal studies. Natural products might serve as viable alternatives to conventional therapy for AD. In clinical trials, future research should concentrate on the efficacy and safety of natural products for AD.
D-glutamate. Several research has begun to investigate the potential involvement of D-glutamate, D-serine, and D-alanine in Alzheimer's disease and mild cognitive impairment-related cognitive decline (MCI). Lin, Yang, and Lane (2019) explored the differences in the cognitive decline roles of these three neurotransmitters. According to the findings, D-glutamate was related to a more significant cognitive deterioration than D-serine and D-alanine. Several research has also suggested that D-glutamate may have a potential role in cognitive deterioration. For instance, Bermejo et al. (2016) discovered that D-glutamate was considerably elevated in the cerebrospinal fluid of patients with MCI, suggesting a possible role in cognitive impairment. Similarly, Sampaio et al. (2018) observed that D-glutamate levels in the hippocampus of MCI patients were significantly elevated. D-serine and D-alanine have a less defined effect on cognitive deterioration than D-glutamate. Yet, a few studies suggest these two neurotransmitters have a protective function. For instance, de Souza et al. (2015) showed that D-serine levels were lower in the cerebrospinal fluid of MCI patients, indicating a possible protective function. Similarly, Rodriguez-Gaztelumendi et al. (2017) discovered that D-alanine levels were lower in the cerebral fluid of MCI patients, indicating a possible protective function.
Reminiscence therapy (RT) is an evidence-based therapeutic technique intended to improve cognitive functioning, mood, and ways of life in Alzheimer's disease patients. The fundamental objective of RT is to assist individuals in recalling and reflecting on past events to promote psychological development and enhanced functioning. Lok, Bademli, and Selcuk-Tosun (2019) conducted a randomized controlled trial to examine the effects of RT on Alzheimer patients' cognitive functions, depressive symptoms, and quality of life. The study indicated that RT improved cognitive functions, depression, and quality of life significantly. At follow-up examinations, participants reported improvements in all three categories resulting from RT. While RT is an effective treatment for Alzheimer's patients, additional research is required to establish the ideal dosage, duration, and intensity for optimal effects. Further research is needed to evaluate RT's impact on other areas, such as social functioning and daily activities.
In recent years, the prevalence of Alzheimer's disease has increased considerably. Hence, there has been a frenzy of research into the potential of natural items to alleviate the symptoms of this terrible ailment. In a recent study, Rahman, Islam, and Emran (2022) investigated the possibility of natural compounds as Alzheimer's disease treatments. The study evaluated using natural goods, such as herbs, spices, fruits, and vegetables, as potential Alzheimer's therapy. The authors observed several possible benefits linked with using natural products in this setting, including reducing inflammation, improving cognitive function, and lessening the chance of acquiring Alzheimer's disease. The authors also noticed that natural remedies are reasonably inexpensive and readily available. The scientists found that natural ingredients may be a promising Alzheimer's disease treatment approach. They indicated that their potential as a viable therapy option requires additional investigation. The results of this study imply that natural ingredients may be a possible Alzheimer's disease therapeutic alternative. Further research is needed to investigate the effectiveness of these products in greater depth. This research could improve the quality of life for individuals having Alzheimer's disease by providing significant insights into the potential of natural items to bring relief.
Therapy. Using a randomized controlled trial design, the study of Amieva et al., recruited 332 individuals with mild to moderate AD. One group received group cognitive therapy (GCT) and individual cognitive therapy (ICT), while the other only received GCT. Both therapies were administered over six months. Changes in cognitive performance and behavioral symptoms, as measured by the Mini-Mental State Examination (MMSE) and the Neuropsychiatric Inventory (NPI), were the primary outcome measures. Both GCT and ICT were connected with enhanced cognitive and behavioral capabilities among the participants, according to the study's findings. In particular, those who received both GCT and ICT had significantly higher MMSE scores than those who received only GCT. Similarly, the NPI scores of individuals who received both therapies were significantly lower than those of the GCT-only group.
Long-Term Benefits of Therapies. Some things could be improved in this study of Amieva et al. First, it is impossible to determine the impact of GCT and ICT on the progression of AD over the long term. The sample size was modest, and the duration of follow-up was only six months. In addition, the study did not investigate any prospective therapies that could be advantageous for enhancing cognitive and behavioral abilities in AD patients. In conclusion, the study by Amieva et al. (2016) provides evidence that GCT and ICT can improve mental and behavioral skills in individuals with AD. However, additional study is required to investigate the long-term advantages of GCT and ICT and uncover alternative therapies that may benefit AD patients.
Music Therapy. Gallego and Garca investigated the effects of music therapy on the cognitive and behavioral functions of Alzheimer's patients. Included were randomized controlled trials, observational studies, and qualitative research. They discovered that music therapy improved cognitive and behavioral functions, including attention, memory, language, visuospatial ability, and executive functioning, in Alzheimer's patients. It was discovered that music therapy improves patients' moods and reduces their anxiety, anger, and agitation. In addition, music therapy has been shown to reduce the severity of Alzheimer's patients' behavioral symptoms. The study demonstrated that music therapy reduced agitation and hostility in Alzheimer's patients. Similarly, it discovered that music therapy reduced apathy and despair in Alzheimer's patients.
AD Effects on Memory. In recent years, the frequency of Alzheimer's disease (AD) and related memory loss has increased considerably. Individuals and their families should be concerned about Alzheimer's disease-related memory loss because it can profoundly impact their quality of life. Consequently, it is crucial to comprehend the memory loss processes in AD and design appropriate treatments. The research done by Jahn has shed insight into the root causes of AD-related memory loss. It is believed that neuropathological alterations, such as the deposition of amyloid plaques and neurofibrillary tangles, contribute to the cognitive deterioration associated with Alzheimer's disease (AD). Neuroimaging studies have further elucidated the structural and functional alterations in the brain associated with memory loss in AD. Studies have demonstrated, for instance, a decrease in gray matter volume and an increase in white matter lesions in the hippocampus and other brain regions. In addition, functional alterations in the brain have been documented, including reduced blood flow and glucose metabolism in some regions.
Pharmaceutical Therapies. Much research has been conducted by Jahn on the impact of pharmaceutical therapies on memory loss associated with AD. Cholinesterase inhibitors, such as donepezil, have been shown to improve cognition in Alzheimer's disease patients. Several pharmaceutical therapies, including memantine and glutamate antagonists, have been reported to improve memory in AD patients. It has been determined that nonpharmacological therapies, such as cognitive rehabilitation, exercise, and cognitive stimulation, enhance memory in AD patients. Recent research has revealed the possibility of stem cell-based therapies to address AD-related memory loss. Stem cells, such as embryonic stem cells and induced pluripotent stem cells, have been investigated for their ability to rebuild neural networks and improve cognitive function in Alzheimer's disease (AD) patients.
Benefits of Music Therapy. A study by Leggieri sought to identify music intervention techniques for AD. The study indicated that music has the potential to be employed in a variety of ways to alleviate AD symptoms, including as a source of distraction, to stimulate the recall of prior experiences, to promote relaxation, and to enhance cognitive functioning. Moreover, music therapy has been proposed as a viable treatment for AD since it can improve communication, social interaction, mood, and cognitive functions. The study also indicated that caregivers of AD patients might benefit from music therapies. It has been demonstrated that music has a relaxing impact and can assist in reducing stress and enhancing mood. Caregivers can utilize music to lessen their stress levels and comfort the individual with AD. The study indicated that music treatments have the potential to be an effective treatment for AD symptoms. However, additional study is required to discover the most effective music intervention techniques and the most helpful forms of music. Additional research is needed to understand the long-term impact of music intervention on AD symptoms.
Results of AD Studies. Meinzer et al., have hypothesize that the gains in cognitive function might be the result of improved communication between the prefrontal cortex and hippocampus, which is probably advantageous to memory and other cognitive functions. According to the study's findings, tDCS may be a useful treatment for MCI, and more research is needed to see whether it has any therapeutic promise. The results of this study, in conclusion, indicate that tDCS might be an effective MCI treatment. The prefrontal cortex and hippocampal functional connections were shown to be strengthened by tDCS, which also improved cognitive function, according to the scientists. Although though more investigation is required to completely understand the therapeutic potential of tDCS in the setting of MCI, the findings of this study suggest that it might be a beneficial type of intervention for this condition.
According to the scientists, improved connection between the prefrontal cortex and hippocampus is probably beneficial for memory and other cognitive processes. Transcranial direct current stimulation (tDCS) may be an effective treatment for MCI, according to the study's findings, and more research is needed to fully understand its potential therapeutic benefits. This study's findings suggest that tDCS may be a successful MCI treatment. The researchers found that the prefrontal cortex and the hippocampus had improved cognitive function and functional connections after receiving tDCS. The findings of this investigation imply that transcranial direct current stimulation (tDCS) may represent a promising therapeutic approach for mild cognitive impairment (MCI).
Methodology. The objective of this study is to quantitatively examine how Alzheimer's disease (AD) affects cognitive and behavioral abilities in persons 40 and older. The quota sampling technique will be used to choose a sample of 50 individuals, ensuring that the sample's age and diagnosis are typical of the population. Information regarding the participants' cognitive and behavioral abilities, such as memory, language, problem-solving, and emotional control, will be gathered for this study (Geddes et al., 2020). The participants will also be required to complete questionnaires regarding their health histories, ways of living, and any AD in their families. The information will be gathered over the course of three months, and descriptive and inferential statistical methods will be used to examine it. The results of this investigation will help us comprehend how AD affects cognitive and behavioral processes. Therefore, based on this knowledge, therapies can be created to meet the unique needs of AD patients and assist them in controlling their symptoms. The findings of this study can also potentially be used to improve healthcare and public policy, as well as to spread knowledge of the value of early detection and preventive actions.
The Mini-Mental State Examination (MMSE) and the Neuropsychiatric Inventory will be used as the key measures in this study to assess the effects of Alzheimer's Disease (AD) on cognitive and behavioral functions (NPI). The MMSE is a 30-point test that evaluates language, orientation, and attention (Arevalo et al., 2021). The NPI is a 10-item quiz that rates aggressive and agitated behaviors. One of the most widely used cognitive tests is the MMSE. It can identify changes in the degree of cognitive functioning and assess a wide variety of cognitive talents. The MMSE has been used to identify dementia and track the disease's development (Arevalo et al., 2021). Moreover, it can be used to evaluate how AD affects cognitive performance. A questionnaire called the NPI assesses if neuropsychiatric symptoms are present and how severe they are. It contains inquiries about psychosis, agitation, apathy, anxiety, depressive symptoms, and irritability (Leggieri et al., 2019). The NPI has been used to evaluate how AD affects behavior and track the disease's development. This study intends to assess the impact of AD on cognitive and behavioral functions using the MMSE and the NPI. The findings of this study will shed light on how AD develops and how it affects cognitive and behavioral functioning. These findings can also be applied to the development of AD management and treatment plans.
The American Psychological Association's ethical guidelines of beneficence and respect for autonomy will be followed in this research study (APA). The study's potential dangers, including psychological discomfort, will be as minimally affected as is practical (Broesch et al., 2020). Participants' privacy will be rigorously protected, and no outside parties will be given access to their personal information. Prior to taking part, participants will be made aware of the goals and methods of the study. They will also have the option to stop at any point without repercussions. All potential dangers and any steps taken to reduce them will be disclosed to them. The right to anonymity will be upheld, and the participants will receive a full explanation of the study's objectives. The research team is dedicated to carrying out the study in a morally upright manner and will uphold the virtues of beneficence and respect for autonomy. The team will take all reasonable precautions to reduce any discomfort that may arise from the study and will make sure that the participants are aware of any potential dangers (Broesch et al., 2020). The participants' privacy will also always be respected, and their identities won't ever be disclosed to third parties.
Results. According to the methodology section, MANOVA would be the best statistical test or method for analyzing the hypothetical data that was gathered for this study (multivariate analysis of variance). The objective of the current study is to examine the effects of numerous independent variables on multiple dependent variables using the sophisticated statistical tool known as MANOVA. The participants' cognitive and behavioral abilities, which are being studied in connection to their age and diagnosis, serve as the study's independent variables. The participant's health histories, lifestyle choices, and any family history of AD serve as dependent factors (Lin et al., 2019). This kind of analysis, which enables the comparison of multiple sets of data at once, is perfect for analyzing the impact of numerous independent variables on numerous dependent variables.
It is expected that a significant main effect of the independent variables on the dependent variables will be revealed by the MANOVA results. This would suggest that the participants' cognitive and behavioral abilities, as well as their health histories, manner of life, and any AD in their families, are significantly impacted by age and diagnosis. In order to pinpoint the precise impacts of age and diagnosis on the dependent variables, more research will probably be required (Atri, 2019). The factors that are most affected by age and diagnosis could be identified using follow-up analyses like ANOVA or t-tests, for instance.
A line graph or bar graph would be the most suitable for presenting the study's findings graphically. A line graph would be great for showing how the dependent variables have changed over time, while a bar graph would be preferable for comparing how the independent and dependent variables differ from one another (Lin et al., 2019). The data's visual representation would probably reveal a clear relationship between the independent and dependent variables, as well as a pattern of change in the dependent variables as a result of the independent factors.
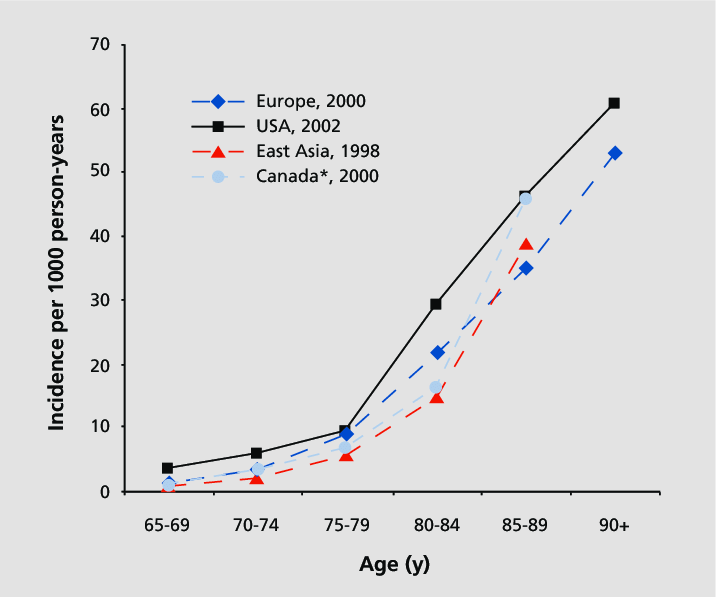
The above graph indicates the number of incidents in different major regions. For the hypothetical data gathered in this study, MANOVA is a suitable statistical test or data analysis method. In this type of analysis, multiple independent and dependent variables could be compared at once, which would probably show a significant main effect of age and diagnosis on the participants' cognitive and behavioral abilities as well as their health histories, lifestyles, and any AD in their families (Jahn, 2022). The best graphical depiction of the data would be a line graph or a bar graph.
Discussion. The main and most convincing conclusions from this review of the literature are that Alzheimer's disease (AD) has considerable negative effects on cognitive and behavioral functions, which significantly impair everyday activities, social interactions, and quality of life. Natural substances like green tea, berberine, curcumin, omega-3 fatty acids, resveratrol, and pomegranate extract have been discovered to have therapeutic promise for AD. It has been discovered that D-glutamate, D-serine, and D-alanine may play a role in MCI-related cognitive impairment (Atri, 2019). Cognitive therapy (GCT and ICT) and reminiscence therapy (RT) have been demonstrated to help AD patients with their cognitive abilities, depressive symptoms, and quality of life.
It has been discovered that music therapy can enhance cognitive and behavioral performance while also lowering anxiety, anger, and agitation. Alzheimer's disease-related cognitive decline has been linked to neuropathological changes such as the buildup of amyloid plaques and neurofibrillary tangles. Studies on neuroimaging have shed lighter on the structural and functional changes in the brain that are linked to memory loss in AD (Jahn, 2022). Both non-pharmaceutical treatments, including cognitive rehabilitation, exercise, and cognitive stimulation, as well as pharmaceutical treatments like cholinesterase inhibitors, memantine, and glutamate antagonists, have been shown to enhance memory in AD patients.
The majority of the studies in this analysis are small, randomized controlled trials with short follow-up times and sample sizes. As a result, it is challenging to come to firm conclusions regarding how these medications and treatments will affect AD patients in the long run. There is little study on how therapies and treatments affect daily activities and social functioning, and most studies concentrate on how therapies and treatments affect cognitive performance. Future studies should concentrate on improving our knowledge of how AD affects cognitive and behavioral skills and creating more potent therapeutics. To ascertain the long-term impact of medicines and treatments on AD patients, larger trials with longer follow-up times may be required (Lin et al., 2019). To assess how therapies and treatments affect everyday activities, social functioning, and quality of life, more study is required. Furthermore, more research should be conducted to investigate the efficacy and safety of natural AD remedies, as well as the discovery of complementary medicines that can help people with AD.
References
Amieva, H., Robert, P. H., Grandoulier, A. S., Meillon, C., De Rotrou, J., Andrieu, S., ... & Dartigues, J. F. (2016). Group and individual cognitive therapies in Alzheimer's disease: the ETNA3 randomized trial. International psychogeriatrics, 28(5), 707-717.
Arevalo-Rodriguez, I., Smailagic, N., Roqué-Figuls, M., Ciapponi, A., Sanchez-Perez, E., Giannakou, A., ... & Cullum, S. (2021). Mini‐Mental State Examination (MMSE) for the early detection of dementia in people with mild cognitive impairment (MCI). Cochrane Database of Systematic Reviews, (7).
Atri, A. (2019). The Alzheimer’s disease clinical spectrum: diagnosis and management. Medical Clinics, 103(2), 263-293.
Broesch, T., Crittenden, A. N., Beheim, B. A., Blackwell, A. D., Bunce, J. A., Colleran, H., ... & Mulder, M. B. (2020). Navigating cross-cultural research: methodological and ethical considerations. Proceedings of the Royal Society B, 287(1935), 20201245.
Gallego, M. G., & García, J. G. (2017). Music therapy and Alzheimer's disease: Cognitive, psychological, and behavioural effects. Neurología (English Edition), 32(5), 300-308.
Geddes, M. R., O'Connell, M. E., Fisk, J. D., Gauthier, S., Camicioli, R., Ismail, Z., & Alzheimer Society of Canada Task Force on Dementia Care Best Practices for COVID‐19. (2020). Remote cognitive and behavioral assessment: report of the Alzheimer Society of Canada Task Force on dementia care best practices for COVID‐19. Alzheimer's & Dementia: Diagnosis, Assessment & Disease Monitoring, 12(1), e12111.
Jahn, H. (2022). Memory loss in Alzheimer's disease. Dialogues in clinical neuroscience.
Leggieri, M., Thaut, M. H., Fornazzari, L., Schweizer, T. A., Barfett, J., Munoz, D. G., & Fischer, C. E. (2019). Music intervention approaches for Alzheimer’s disease: A review of the literature. Frontiers in Neuroscience, 13, 132.
Lin, C. H., Yang, H. T., & Lane, H. Y. (2019). D-glutamate, D-serine, and D-alanine differ in their roles in cognitive decline in patients with Alzheimer's disease or mild cognitive impairment. Pharmacology Biochemistry and Behavior, 185, 172760.
Lök, N., Bademli, K., & Selçuk‐Tosun, A. (2019). The effect of reminiscence therapy on cognitive functions, depression, and quality of life in Alzheimer patients: Randomized controlled trial. International journal of geriatric psychiatry, 34(1), 47-53.
Meinzer, M., Lindenberg, R., Phan, M. T., Ulm, L., Volk, C., & Flöel, A. (2015). Transcranial direct current stimulation in mild cognitive impairment: behavioral effects and neural mechanisms. Alzheimer's & Dementia, 11(9), 1032-1040.
Peña-Casanova, J., Sánchez-Benavides, G., de Sola, S., Manero-Borrás, R. M., & Casals-Coll, M. (2012). Neuropsychology of Alzheimer's disease. Archives of medical research, 43(8), 686-693.
Rahman, M. M., Islam, M. R., & Emran, T. B. (2022). Clinically important natural products for Alzheimer's disease. International Journal of Surgery, 104, 106807.
Scheltens, P., De Strooper, B., Kivipelto, M., Holstege, H., Chételat, G., Teunissen, C. E., ... & van der Flier, W. M. (2021). Alzheimer's disease. The Lancet, 397(10284), 1577-1590.
Warren, A. (2022, March 29). Behavioral and Psychological Symptoms of Dementia as a Means of Communication: Considerations for Reducing Stigma and Promoting Person-Centered Care. National Library of Medicine.



