M4_A1
In Module 4, you will focus on treatment and intervention strategies geared toward stabilization. The first stage in stabilization involves correctly naming the problems and restoring a sense of control to the patient by providing the individual with a sense of safety in the room with you and in the process of therapy. After the experience of trauma, a victim may feel out of control, helpless, and hopeless. If these feelings continue and grow stronger, the likelihood increases that the victim may fall into depression and perhaps display suicidal behavior. This is a key reason why immediate intervention and instilling a sense of universality and hope are so important. Victims need to be made to feel that they are not alone, their experiences are not unique, and their circumstances are survivable.
An important part of the skills you will develop in designing appropriate interventions is the ability to design a treatment plan focused on stabilization appropriate for the particular client being treated. It is important to keep in mind that victims' responses vary widely, and it is imperative that treatment planning and approaches be individualized to the specific victim's needs. In this module, you will create a treatment plan for stabilization based on the information provided in the case study. Additionally, you will discuss the effects of child sexual abuse on emotion.
Identify and evaluate commonalities and differences in demographic variables and psychological profiles between subtypes of victims that may present in forensic settings.
Compare and contract empirical research findings for related to treatment for victims.
Please view Treatment Relationship
Safety
Creating safety for the client is the first of three stages outlined by Herman as necessary for the treatment of trauma survivors. The first stage involves correctly naming the problems and restoring a sense of control to the survivor by providing the survivor with a sense of safety in the room with you and in the process of therapy. The second stage, remembrance and mourning, and the third stage, reconnection and thriving, will be covered in the next module.
Some thoughts about safety:
Patients are not likely to feel safe until they are in control of their symptoms, and a therapist will not be able to help clients achieve control over their symptoms if the therapist has not properly assessed the patients. Thus, the first goal within the safety stage is assessment, which is as follows:
This means getting a thorough history of the presenting issue and anchoring it in measurable terms. For example, you might say to the client, "Describe your panic on a scale of one to ten and explain how difficult it is to get to work now, as compared to six months ago." Conducting an assessment allows the client to explain the symptoms being experienced on an easy-to-comprehend scale and allows the therapist and the client to quickly create a shared understanding as to the client's experience.
You are there to assess not only problems but also strengths. When assessing for problems and strengths, you will explore feelings, thoughts, and behaviors. It is very important to model the exploration of strengths from the very beginning of treatment. If the client is unable to name any area of strength, you may ask what other people in the person's life have described as strengths in the individual, or you may name qualities you have noticed, and then encourage the client to name one. One of the advantages of strengths-based intervention is that it teaches clients to believe and trust in their own abilities, to navigate their environments successfully, and to envision a life for themselves beyond their immediate experience of posttrauma pain.
Unlike some traditional medical models, the trauma model is going to keep coming back to the idea of empowerment and assuming the victims have within themselves the best solutions. The therapist will work with the clients to help them regain access to those parts of themselves—so you will want to be sure to focus on strengths, too! For example, "We have spent some time talking about problems you are having currently; however, I get the sense you have been doing some things to help yourself already. Tell me what things you have tried that haven't helped at all, as well as things you do that reduce your feeling of panic or have helped you with anxious situations in the past." These types of statements help a client to remember a time when he or she felt more competent and in control and instill a sense of hope that such a state can be rediscovered.
The Diagnostic and Statistical Manual of Mental Disorder (DSM) states differential diagnosing is also going to be an aspect of this step. Keep in mind that not all survivors of trauma will have posttraumatic stress disorder (PTSD), but they may have other maladaptive coping methods, resulting in another diagnosis (such as agoraphobia, depression, or substance abuse).
Be sure to assess social support as part of the assessment phase. In trauma cases in particular, the presence or absence of a supportive family, friends, religious community, work environment, or a partner (among others) often has a dramatic impact on the recovery, and you need to take this into consideration as you develop the treatment plan and discuss coping skills. In addition, intervention may be offered to family members, especially domestic partners, who may be struggling with their own feelings regarding what has happened to their loved ones. Family members of survivors can benefit from being educated about types of trauma and common reactions, self-care strategies, and also how best to be a source of support to the survivors.
Restoring Control
Once the primary presenting issues are identified, you can begin to help the patient to regain control over the most troubling aspects immediately—the ones getting in the way of the individual's functioning. This process can take days, weeks, or even years, but it should always be part of the starting point.
In this step of gaining safety, you work with the individual to help the patient regain control over his or her body, over the immediate environment, and the larger community. Picture a series of circles inside each other. You are going to help the patient take control from the inside to the outside.
You begin by helping the client establish a routine in self-care of such aspects as sleep, nutrition, and exercise, which often are not taken care of adequately in mental health realms. However, especially in cases in which the violation has been physical, resuming control of this part of a person's life can be very empowering.
Some examples of interventions include working with a client on deep-breathing exercises, muscle relaxation, and visualization techniques and developing a list of strategies to deal with anxiety, depression, sleeplessness, panic, or rage—all with the goal of helping the client get the most troubling symptoms out of the way so the individual can function adequately in his or her day-to-day life.
Convincing a client to buy into an individualized goal can be an important step toward making immediate progress toward restoring previous functioning. Examples of goals might be that the client will take a ten-minute walk in the neighborhood each day or will drive to work on time and stay all day at work as scheduled. As the survivor is able to master these smaller goals, more advanced goals can take their place.
All these interventions need to happen before the second stage of treatment.
Measurement Tools
The National Center for PTSD lists more than seventy assessment tools for measuring PTSD (US Department of Veterans Affairs, n.d.). Information on each tool is available to the general population. Information on how to obtain the assessments is provided for qualified mental health practitioners. We have discussed that assessments and interventions should be selected on a case-by-case basis taking into consideration the presenting issues of the individual survivor. For example, not all survivors will experience immediate anxiety following a traumatic event. The selection of assessment measures may be influenced by a survivor's age, clinical presentation, self-report, existing support system, and current mental status and survivor status reports made by family members.
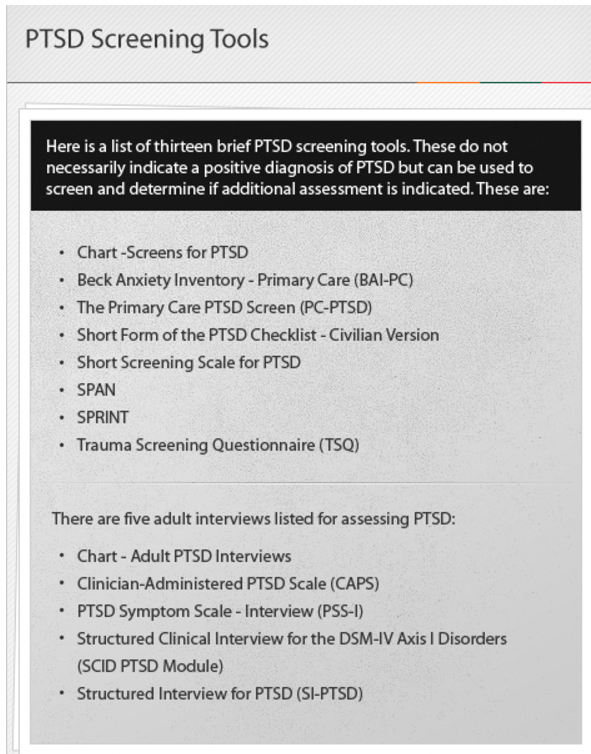
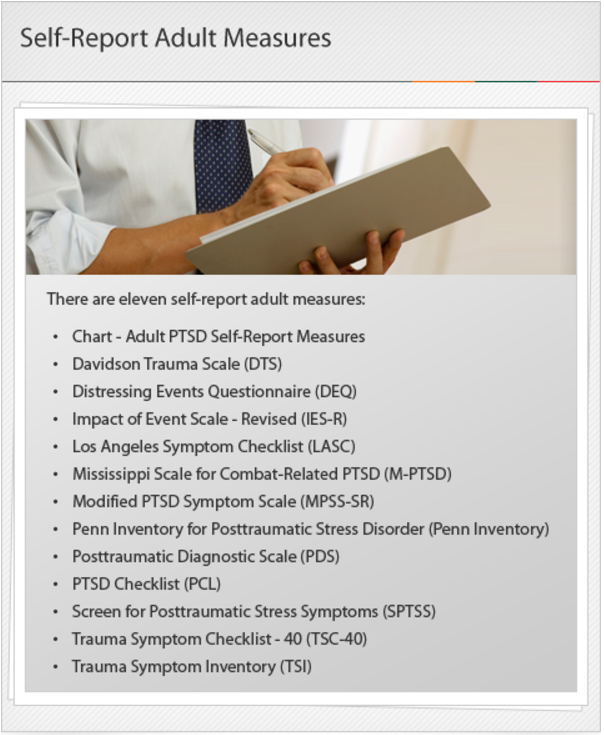 With the plethora of assessment tools out there, a practitioner should become familiar with those measures that are a best fit for the populations to which he or she provides services.
With the plethora of assessment tools out there, a practitioner should become familiar with those measures that are a best fit for the populations to which he or she provides services.
Reference:
US Department of Veterans Affairs. (n.d.). PTSD: National Center for PTSD:
List of all measures. Retrieved from http://www.ptsd.va.gov/professional/
assessment/all_measures.asp
Conclusion
In this module you learned a great deal about assessment and evaluation of victims. Some of the topics that you learned more about included:
Differential diagnosis process
Complex PTSD
Measurement tools
Revictimization, risk variables, and the cycle of violence
Understanding these issues is essential to the treatment process, which includes diagnosis and assessment.



