HCA415 Community & Public Health-WK2-A1
5.1 Introduction
The previous chapters provided information on the basic concepts of community and public health; for example, history, definitions of terms, and epidemiology. Chapter 5 covers the broad topic of maternal, infant, and child health, including the health of teenagers. Infants, children, and teenagers are a demographically important group that forms a large percentage (nearly one-quarter of the total population) of the United States. In 2010, 74.2 million persons were under the age of 18 years (Howden & Mayer, 2011).
Healthy People 2020 states that
[t]he well-being of mothers, infants, and children determines the health of the next generation and can help predict future public health challenges for families, communities, and the medical care system. Moreover, healthy birth outcomes and early identification and treatment of health conditions among infants can prevent death or disability and enable children to reach their full potential. (HealthyPeople.gov, 2013b)
One of the crucial dimensions of maternal, infant, and child health is family planning and the empowerment of women regarding fertility and childbirth. This is the first topic discussed in the chapter. Significant community health issues associated with the unavailability of family planning services are high levels of infant mortality and mothers' inability to use prenatal health care services. Family planning services can help contribute to good birth outcomes as well as healthy babies and children. Unfortunately, limited availability of family planning services and low utilization of prenatal care can lead to infant mortality.
In comparison with many other developed countries, the United States ranks high with respect to infant mortality. In 2008, with respect to its infant mortality rate, this nation was in 28th position among a group of 31 of the world's developed nations (USDHHS, 2013). At that time, the U.S. infant mortality rate was more than twice the rate in Sweden, the country with the lowest rate. The respective figures were 6.6 per 1,000 (United States) versus 2.5 per 1,000 (Sweden).
What accounts for the low international standing of the United States with respect to infant mortality, and what are some of the causes of infant mortality? This chapter will point out that America faces many disparities in infant mortality across racial and economic divides. These disparities are reflected in the occurrence of adverse birth outcomes, such as preterm births, and infant deaths from causes such as sudden infant death syndrome.
Adverse birth outcomes are determinants of subsequent infant health. Factors associated with such outcomes are alcohol consumption, cigarette smoking, and prescription and nonprescription drug use during pregnancy. In addition to family planning, methods for reducing adverse birth outcomes include maternal health promotion through good nutrition, avoidance of smoking and alcohol consumption, breastfeeding during infancy, and provision of childcare to working mothers.
Photograph of a mother reading to her children.
Fotosearch/SuperStock
Mothers, infants, and children form the bedrock of community health. Their health ultimately determines what the future health of the community will look like.
Although the self-reported health of children in the United States tends to be at a high level—more than 80% of school-age children are in excellent or very good health—many children are afflicted with preventable infectious diseases, chronic diseases, and chronic conditions. Examples of chronic conditions that emerge during childhood are learning disabilities (e.g., Attention Deficit/Hyperactivity Disorders and Autism Spectrum Disorders). Also, a significant level of mortality from chronic diseases, preventable infectious diseases, and unintentional injuries occurs during childhood in the United States.
The teenage years are a time for new onset of chronic diseases and adoption of behaviorally linked disease risk conditions. Significant health issues for this group are teenage pregnancy, chronic diseases such as cancer, unintentional injuries, interpersonal violence, suicide, and conditions associated with an adverse lifestyle.
Healthy People 2020: Maternal, Infant, and Child Health—An Overview
Chapter 1 introduced Healthy People, which formulates a science-based strategy for improving our nation's health by the end of the 21st century. During the 3 decades since the beginning of Healthy People, three major publications (Healthy People 2000, Healthy People 2010, and Healthy People 2020) have presented goals for improving Americans' health. Healthy People 2020 objectives stress the importance of maternal and child health for the health of the nation (HealthyPeople.gov, 2012c). The goal of Healthy People 2020 in this arena is to: "Improve the health and well-being of women, infants, children, and families" (para. 2) The objectives of the maternal, infant, and child health topic area address a wide range of conditions, health behaviors, and health systems indicators that affect the health, wellness, and quality of life of women, children, and families. For more information, see Health Care in Action: Healthy People 2020: Summary of Objectives: Maternal, Infant, and Child Health.
Health Care in Action: Healthy People 2020: Summary of Objectives: Maternal, Infant, and Child Health
Number and Objective Short Title
Morbidity and Mortality
MICH–1 Fetal and infant deaths
MICH–2 Deaths among infants with Down syndrome
MICH–3 Child deaths
MICH–4 Adolescent and young adult deaths
MICH–5 Maternal deaths
MICH–6 Maternal illness and complications due to pregnancy
MICH–7 Cesarean births
MICH–8 Low birth weight and very low birth weight
MICH–9 Preterm births
Pregnancy Health and Behaviors
MICH–10 Prenatal care
MICH–11 Prenatal substance exposure
MICH–12 Childbirth classes
MICH–13 Weight gain during pregnancy
Preconception Health and Behaviors
MICH–14 Optimum folic acid levels
MICH–15 Low red blood-cell folate concentrations
MICH–16 Preconception care services and behaviors
MICH–17 Impaired fecundity
Postpartum Health and Behavior
MICH–18 Postpartum relapse of smoking
MICH–19 Postpartum care visit with a health worker
Infant Care
MICH–20 Infants put to sleep on their backs
MICH–21 Breastfeeding
MICH–22 Worksite lactation support programs
MICH–23 Formula supplementation in breastfed newborns
MICH–24 Lactation care in birthing facilities
Disability and Other Impairments
MICH–25 Fetal alcohol syndrome
MICH–26 Disorders diagnosed through newborn bloodspot screening
MICH–27 Birth weight of children with cerebral palsy
MICH–28 Neural tube defects
MICH–29 Children with Autism Spectrum Disorder and developmental delay screening
Health Services
MICH–30 Access to [a] medical home [a "home base" for medical care]
MICH–31 Care in family-centered, comprehensive, coordinated systems
MICH–32 Newborn bloodspot screening and follow-up testing
MICH–33 Very low birth weight infants born at level III hospitals
Source: Reprinted from HealthyPeople.gov. (2012d). Summary of objectives. Maternal, infant, and child health. Retrieved from http://www.HealthyPeople.gov/2020/topicsobjectives2020/pdfs/MaternalChildHealth.pdf
Maternal health refers to the health of women during pregnancy, childbirth, and the postpartum period (CDC, 2012l). The health of mothers is crucial to the overall health of the community and reflects the commitment of society to future generations. The key aspects of maternal health are family planning, the occurrence of maternal mortality and other adverse outcomes during pregnancy, and maternal health promotion. A trend in maternal health (perhaps in response to the growing number of births among older women) is an increasing number of cesarean births in the United States.
Family Planning
Healthy People 2020 states that "family planning is one of the 10 great public health achievements of the 20th century. The availability of family planning services allows individuals to achieve desired birth spacing and family size, and contributes to improved health outcomes for infants, children, women, and families." The goal of Healthy People 2020 with respect to family planning is to "[i]mprove pregnancy planning and spacing, and prevent unintended pregnancy" (HealthyPeople.gov, 2012b, para. 1 & 2). Healthy People 2020 lists the following activities as parts of family planning services:
Contraception and broader reproductive health services
Breast and pelvic examinations
Breast and cervical cancer screening
Sexually transmitted disease (STD) (more commonly known today as sexually transmitted infection [STI]) and human immunodeficiency virus (HIV) counseling
Pregnancy diagnosis and counseling, and screening.
Photograph of a birth control pill container.
iStockphoto/Thinkstock
Family planning methods, such as providing education and access to birth control, seek to support individuals in creating the family they choose at a time that is best for them.
According to the World Health Organization, family planning is a method for helping people to have the desired number of children and for spacing births (WHO, 2012d). In less developed parts of the world, almost 250 million women who do not use any type of contraception would benefit from greater access to methods of family planning. The population growth of some developing countries exceeds the carrying capacity of the local area; more to the point, family planning can be helpful in bringing population in line with the Earth's carrying capacity, improving living conditions, and increasing economic development.
Family planning is essential to the health and autonomy of women, as well as for supporting the health and development of communities. From the world perspective, WHO cites the following advantages of family planning:
May help to prevent the transmission of sexually transmitted infections
Reduces the need for unsafe abortions
Contributes to the health and well-being of women
Aids in delaying pregnancies among very young women who are at risk of complications and death from childbearing
Helps to prevent pregnancies among older women, who are at high risk of complications.
Internationally, organizations such as the Bill and Melinda Gates Foundation support access to family planning services. In the United States, Planned Parenthood and community-based organizations have been involved with family planning. Planned Parenthood provides reproductive health care to men, women, and teens (Planned Parenthood, 2013). A total of 73 Planned Parenthood affiliates are situated in local communities and are responsible for more than 750 health centers. Planned Parenthood indicates that "[t]hese health care centers provide a wide range of safe, reliable health care—and more than 90 percent is preventive, primary care, which helps prevent unintended pregnancies through contraception, reduce the spread of sexually transmitted infections, through testing and treatment, and screen for cervical and other cancers" (Planned Parenthood, 2013; Providing Trusted Community Health Care).
Additionally, The National Family Program was instituted in 1970 as part of Title X of the Public Health Service Act and is operated by the Office of Population Affairs (USDHHS, 2012). Funds from Title X support contraception (with the exception of abortion), family planning, and associated preventive health care. During 2011, Title X funding was awarded to 91 recipients (both public and private) located in the ten United States Department of Health and Human Services Areas. Examples of grantees were state and local health departments, nonprofit organizations, independent service providers, and agencies based in the community. The main grantees reallocated these funds to 1,142 subrecipients, creating a network of more than 4,000 family planning service sites. Programs funded under Title X served more than 5 million clients in 2011.
In order to provide health care services, public health programs utilize community health workers who are often on the front line of contact with members of the community. The Health Resources and Services administration reported that reproductive health concerns—sexually transmitted infections (such as HIV), prenatal care, and family planning—were among the issues covered most frequently by community health workers (Gold, 2010). Thus, community health workers are an important link in the chain of resources for family planning services, especially services for individuals from economically disadvantaged and immigrant communities.
Adverse Maternal Health Outcomes Associated With Pregnancy
Examples of adverse maternal health outcomes associated with pregnancy are maternal mortality and depression. Health promotion programs can aid in producing optimal health of pregnant women and their newborn infants. Healthy newborn children have an increased likelihood of progressing toward a healthy childhood and adolescence and becoming healthy adults. The definition of a pregnancy-related death is "the death of a woman while pregnant or within one year of pregnancy termination regardless of the duration or site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes" (CDC, 2012g, para. 1). Maternal mortality is considered a largely preventable condition and reflects the operation of environmental factors and the quality of health care. In less developed areas of the world, maternal mortality is many times higher than in wealthy countries.
Photograph of a pregnant Black woman sitting near a window.
Cusp/SuperStock
Marital status is just one of the factors linked to higher risk of maternal mortality among Black women. Statistically, single black women run a higher risk of maternal mortality than married white women.
Maternal Mortality (Pregnancy Associated Mortality)
Maternal mortality in the United States has been increasing during recent years. Although the reasons for this increase are not entirely clear, researchers have hypothesized that it may be associated with a number of factors. These are improved reporting systems for maternal mortality, the influence of a greater number of chronic conditions among pregnant women, adverse social conditions, lack of utilization of prenatal and postnatal care, and quality of care rendered during the birth process. For example, chronic diseases such as diabetes and hypertension can increase the risks of maternal mortality. In addition, pregnant women who do not receive any prenatal care or limited prenatal care have greater risks for undetected diseases and conditions that can also result in maternal mortality. A total of more than 70% of cases of maternal mortality can be attributed to the following seven causes: hemorrhage, thrombotic pulmonary embolism, infection, hypertensive disorders, cardiomyopathy, cardiovascular conditions, and noncardiovascular medical conditions (Berg et al., 2010). Figure 5.1 presents 10 leading causes of pregnancy-related death in the United States, for 2006–2008. The four leading causes shown in the figure were cardiovascular diseases, cardiomyopathy, noncardiovascular diseases, and hemorrhage.
The maternal mortality rate is defined as the number of deaths per 100,000 live births that are assigned to causes related to pregnancy. A total of 548 women died in the United States in 2007 from pregnancy-related causes (USDHHS, 2011); the highest rate (34.8 per 100,000) occurred among Black women. This rate has tended to increase in the United States during the past 2 decades. In 2007, the maternal mortality rate was 12.7 per 100,000 live births. This number represented approximately a twofold increase in comparison with 1987, when the rate was 6.6 per 100,000. The maternal mortality rate in California, the most populous state in this country, also showed an increasing trend. The rate for California (12.2 per 100,000 live births) between 2007 and 2009 was similar to the national rate for 2007 (California Department of Public Health, 2012). The Center for Family Health, Maternal, Child, and Adolescent Health located in the California Department of Public Health gives several possible explanations for this increase. These include "improved vital statistics data reporting, increasing prevalence of chronic conditions among pregnant women, worsening negative impact of social determinants of health, and quality of care issues in the prenatal period, at the time of labor and delivery, or in the postpartum period" (California Department of Public Health, 2012, p.1). The findings from the California Department of Public Health raise concerns about racial and social differences in maternal mortality.
There are substantial racial disparities in pregnancy-related mortality. The rate for Black women tends to be about three times the rate for White women (CDC, 2012g). The rates for the years 2006 and 2007 were as follows:
11.0 deaths per 100,000 live births for White women
34.8 deaths per 100,000 live births for Black women
15.7 deaths per 100,000 live births for women of other races.
In addition to race, factors associated with maternal mortality are older age of the mother, marital status, and not having access to prenatal care. Between 1998 and 2005, unmarried White women had a 40% higher level of maternal mortality than married White women (Berg et al., 2010).
Figure 5.1: Causes of pregnancy-related death in the United States, 2006–2008
A bar graph showing the percentage of pregnancy-related deaths caused by conditions such as cardiovascular disease, hemorrhage, and anesthesia complications, amongst other causes. Cardiovascular diseases and cardiomyopathy are the top causes of death, with 13.5 and 12.6% of the deaths, respectively. Hemorrhages, noncardiovascular disease, hypertension and other pregnancy disorders, infection, and thrombotic pulmonary embolisms each are responsible for about 11% of pregnancy-related deaths. Anesthesia complications rank the lowest, with 0.6% of the reported deaths.
Source: Adapted from CDC. Retrieved from http://www.cdc.gov/reproductivehealth/MaternalInfantHealth/Pregnancy-relatedMortality.htm
It is important for pregnant women to maintain a healthy lifestyle while pregnant, as well as seek consistent prenatal care, to prevent pregnancy-related conditions.
Depression During and After Pregnancy
Another health event that sometimes occurs during and after pregnancy is depression. This is a fairly common phenomenon that affects about one-twelfth of pregnant women (USDHHS, 2009a). A symptom of depression is feeling sadness and hopelessness during pregnancy. Possible causes of depression are a family history of depression, changes in brain chemistry, stress, and hormonal influences during pregnancy. Postpartum depression, a serious form of depression that occurs after childbirth, is believed to be associated with the rapid return of hormones to normal levels; treatment is imperative for postpartum depression. "Baby blues" are a milder and self-limited form of mood disturbance than postpartum depression. Affected women who do not seek treatment for serious depression can increase the risk of adverse effects upon their own health and the health and development of their fetus and newborn infant. Among the examples of harm to children linked to postpartum depression was the 2010 case of a South Carolina woman, Shaquan Duley, who confessed to drowning her two children in a river and was believed possibly to have been afflicted with postpartum depression.
Cesarean Births
Cesarean delivery (c-section) is "the delivery of the fetus by surgical incision through the abdominal wall and uterus (from the belief that Julius Caesar was delivered in this manner)" (The Free Dictionary, 2013). This method of delivery is regarded as major surgery. Some of the medical indications for cesarean delivery are "[r]epeat cesarean delivery, . . . [o]bstructive lesions in the lower genital tract, . . . [and p]elvic abnormalities" (Medscape Reference, 2011). Nonmedically indicated or elective cesarean delivery is a controversial topic with respect to its risks and benefits. A nonmedically indicated procedure in this instance is one that is not required for maintaining the health and safety of the mother or her fetus. The disadvantages of nonmedically indicated cesarean delivery are higher rates of complications, more frequent rehospitalization of mothers, and neonatal complications. Also, cesarean delivery is more costly than vaginal delivery.
Between 1996 and 2007, the rates of cesarean delivery increased by 53% from 21 per 100 to 32 per 100 births, or about one-third of all births in the United States (Menacker & Hamilton, 2010). The percentage in 2007 was the highest ever recorded up to that time. From 1996 to 2007, the rates of cesarean deliveries tended to increase with increasing age group. In 2007, the highest rates (48% of all births) occurred among women aged 40 to 54 years.
Often, there are specific medical indications for cesarean delivery. However, the increasing trend also is associated with nonmedical factors that include convenience in scheduling a birth (which is normally unpredictable), fear regarding the childbirth process, worry about possible physical damage caused by a vaginal delivery, and legal considerations (e.g., concerns about legal liability). For example, litigation could occur when a cesarean delivery might have prevented an adverse birth outcome.
Maternal Health Promotion and Prenatal Health Care
Health System Indicators
Dr. Novotny discusses infant and maternal health, and their importance in assessing the overall community health.
Critical Thinking Question:
How can assessing the public health help with chronic diseases, such as Diabetes or obesity? Research the maternal or infant health in your community — what do they indicate about the health of the area?
One of the highest priorities for maternal health promotion is the provision of prenatal care to all pregnant women. Prenatal care affords an opportunity to reduce the risks associated with pregnancy. Healthy People points out that
[t]he risk of maternal and infant mortality and pregnancy-related complications can be reduced by increasing access to quality preconception (before pregnancy), prenatal, and interconception (between pregnancies) care. Moreover, healthy birth outcomes and early identification and treatment of health conditions among infants can prevent death or disability and enable children to reach their full potential. (HealthyPeople.gov, 2012c, para. 5)
Healthy People states that "Pregnancy can provide an opportunity to identify existing health risks in women and to prevent future health problems for women and their children" (healthypeople.gov, 2012c, para. 3). The possible health risks to the pregnant woman and her fetus include a range of conditions such as high blood pressure and heart disease, diabetes, depression, genetically associated diseases, sexually transmitted infections (STIs), smoking, alcohol abuse, prescription and illicit drug use, poor nutrition, and unhealthy weight (HealthyPeople.gov, 2012c). One of the reasons for monitoring prescription and other drug use during pregnancy is the drugs' potential teratogenic effects. A teratogen is a substance that can cause abnormalities in the fetus.
Photograph of prebirth checkups at the Family Health and Birthing Center in Weslaco, Texas.
Karen Kasmauski/Science Faction/SuperStock
Regular prenatal checkups help to ensure the healthy growth of the fetus and continued health of the mother through pregnancy. This photo depicts volunteer midwives from the Family Health and Birthing Center in Weslaco, Texas who commit to about a year of work providing prenatal care to clients from lower income communities.
Prenatal Care
Prenatal care is the health care a woman receives while she is pregnant (USDHHS, 2009b). Important components of prenatal care are periodic visits to health care providers beginning with early pregnancy and maintenance of a healthy diet that provides adequate amounts of folic acid. Such care should begin early during pregnancy and continue on a regular basis in order to provide the greatest benefit. Prenatal care optimizes the health of the pregnant woman and that of her developing fetus. The former Surgeon General of the United States, C. Everett Koop, wrote about the need "to increase the public's understanding of health risks to pregnancy and to motivate pregnant women and women planning a pregnancy to take action to protect their health, obtain regular prenatal care, and seek other assistance when needed" (Koop, 1982).
Postpartum (Postnatal) Care
The term postpartum care refers to care given to new mothers after delivery of a child. Another term for postpartum care is postpregnancy health (United States National Library of Medicine, 2012). The postnatal period denotes the time interval that begins after birth and extends until about the first 6 weeks after birth. This time span is critical to the health and survival of a mother and her newborn. WHO notes that postnatal care is an effective means of preventing newborn deaths (WHO, 2012b). Nevertheless, worldwide, many babies are born outside of a hospital, and 70% of them do not receive any postnatal care.
Maternal and Child Nutrition
Maternal nutrition contributes to the development of healthy infants. During pregnancy, positive aspects of nutritional practices involve folic acid supplementation to prevent birth defects, avoidance of fish that contains mercury, and avoidance of exposures to environmental hazards. Exclusive breastfeeding of infants is a desirable practice that helps to protect the health of babies and benefits the health of mothers and society (USDHHS, 2010).
To reinforce optimal nutrition of infants, WIC encourages breastfeeding of infants. Women, Infants, and Children (WIC) is a special supplemental nutrition program designed for low-income women. The WIC program targets "low-income pregnant, postpartum and breastfeeding women, and infants and children up to age 5 who are found at nutrition risk" (United States Department of Agriculture [USDA], 2011, para. 1). Eligibility requirements vary according to family size and income. In order to be eligible for the program, an applicant's gross income must be at or below 185% of the U.S. poverty level. For example, during 2012 through 2013, that income level was $42,643 for a family of four persons (USDA, 2013).
Annually, federal grants to support the WIC program are awarded to states:
WIC is a Federal grant program for which Congress authorizes a specific amount of funding each year for program operations. The Food and Nutrition Service, which administers the program at the Federal level, provides these funds to WIC State agencies (State health departments or comparable agencies) to pay for WIC foods, nutrition education, breastfeeding promotion and support, and administrative costs. (USDA, 2012)
5.3 Health of Infants
Infant mortality has declined in the United States during much of the past half-century, but more recently has plateaued. The United States has relatively high infant mortality rates in comparison with other developed countries and needs to improve this unfortunate situation. Possible methods for reducing infant mortality are through the application of public health interventions that are known to be effective, and by focusing on racial and ethnic disparities. Many of these interventions need to be directed at improving health-related behaviors among pregnant women and increasing their utilization of prenatal care.
Infant Mortality
Infant mortality is defined as "the death of a baby before his or her first birthday" (CDC, 2012k). The death of an infant is a tragic event for parents and family members and a great loss for the community. This rare occurrence happens in about 6 out of 1,000 births in the United States. Nevertheless, given the large population of this country, approximately 25,000 infants die annually; the total number of infant deaths in 2009 was 26,412. Often, infant mortality is used as an indicator of the health status and social conditions prevailing in a country and for making international comparisons of the quality of health services.

Hemis.fr/SuperStock
Due, in part, to economic disparities among these groups, infant mortality rates in the United States are highest among American Indians/Alaska Natives and non-Hispanic Blacks.
Infant Mortality Rate
Data from the National Center for Health Statistics indicate that the infant mortality rate in the United States in 2011 was 6.05 infant deaths per 1,000 live births (MacDorman, Hoyert, & Mathews, 2013). Since 1940, the infant mortality rate has declined greatly, from almost 50 per 1,000 to slightly more than 6 per 1,000. Infant mortality rates have declined steadily since 1960 when there were 26.0 deaths per 1,000 live births to 6.9 per 1,000 live births in 2000. However, the infant mortality rate showed no decrement between 2000 and 2005 (MacDorman & Mathews, 2008). From 2005 to 2006 the rate again declined, leveled off between 2006 and 2007, and then continued to decline until 2011 (the year for which the latest data are available). As noted previously, the United States has a higher infant mortality rate than most other developed countries. Demographers theorize that among the factors related to the low ranking of the United States are social and economic disparities among ethnic and racial groups, especially among Blacks.
Infant Mortality Disparities and Sociodemographic Variations
In the United States, marked disparities in infant mortality exist among racial and ethnic groups. Refer to Figure 5.2 for 2007 data on infant mortality rates by race and ethnicity of the mother. The figure shows that the rates were highest among non-Hispanic Blacks and American Indians/Alaska Natives and lowest among Asians/Pacific Islanders and persons of Central and South American origin (CDC, 2012n).
Figure 5.2: Total and preterm-related infant mortality rates by race and ethnicity of mother, United States, 2007
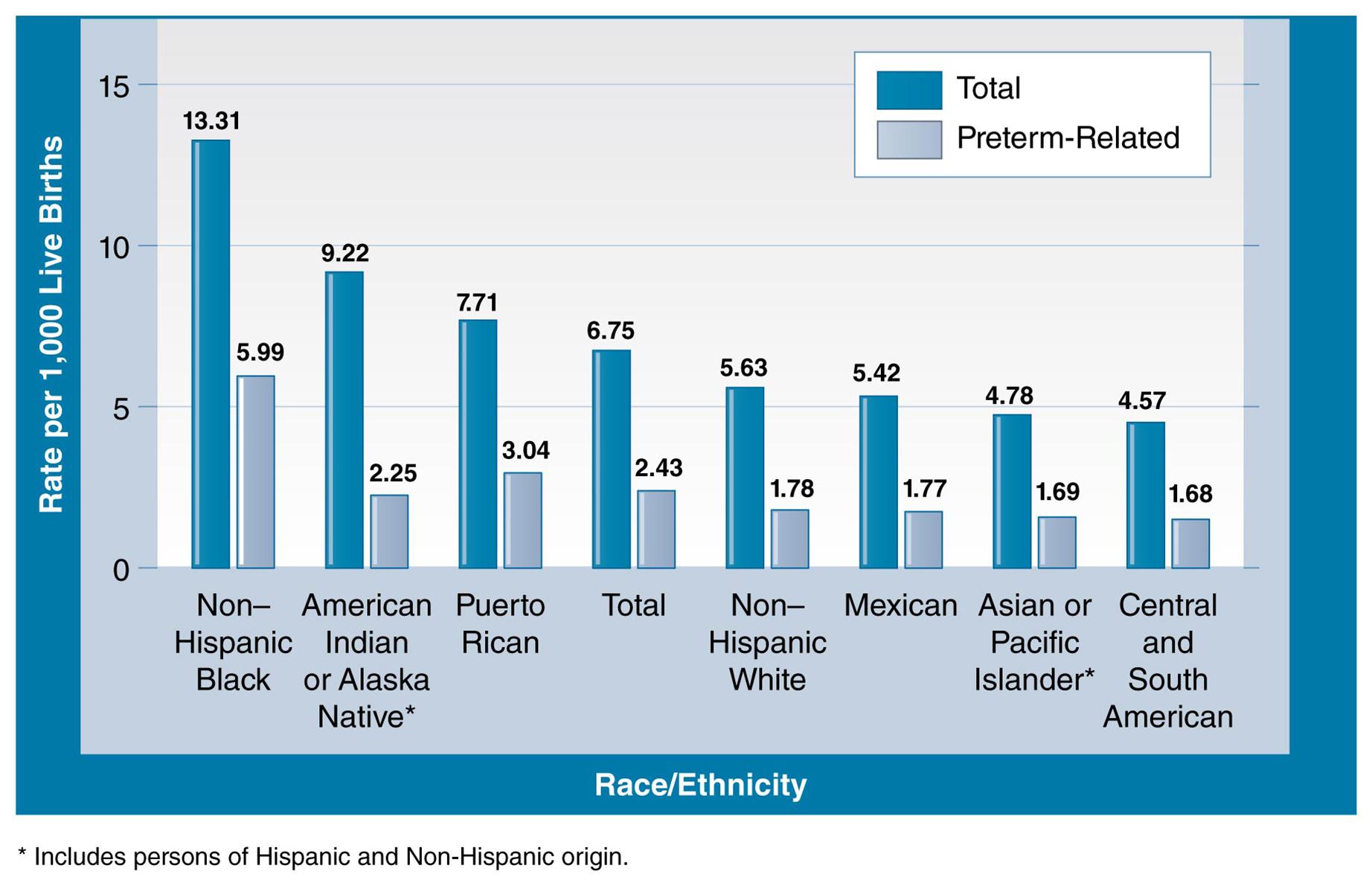
Source: Adapted from CDC. Retrieved from http://www.cdc.gov/reproductivehealth/MaternalInfantHealth/PretermBirth.htm
What might mothers in Central and South America be doing different that lowers their chances of preterm or total infant mortality? What might be affecting the rates of non-Hispanic Black infant mortality?
Data from the Office of Minority Health (OMH) indicate that infant mortality among Blacks is more than two times the rate among non-Hispanic Whites (USDHHS, 2012). In 2008, the infant mortality rate for non-Hispanic Whites was 5.6 per 1,000 live births; for non-Hispanic Blacks, the rate was 13.1 per 1,000 live births. The following facts regarding infant mortality in 2008 among Blacks are from the OMH:
Blacks had twice the sudden infant death syndrome mortality rate as non-Hispanic Whites.
Black mothers were 2.3 times more likely than non-Hispanic White mothers to begin prenatal care in the third trimester, or not receive prenatal care at all.
The infant mortality rate for Black mothers with over 13 years of education was almost 3 times that of non-Hispanic White mothers in 2005.
Other factors related to infant mortality in the United States include the state where the infant was born and maternal education and income (Heisler, 2012). In 2008, the four states with the highest infant mortality rates were Louisiana (9.1 per 1,000), Alabama (9.5 per 1,000), Mississippi (10.0 per 1,000), and South Dakota (8.4 per 1,000). The District of Columbia had a rate of 10.8 per 1,000. The states with the four lowest rates were New Hampshire (4.0 per 1,000), Vermont (4.6 per 1,000), Utah (4.8 per 1,000), and California and Massachusetts (both tied in fourth place with 5.1 per 1,000).
Higher levels of parental education and income are related to lower rates of infant mortality (Heisler, 2012). For example, rates of infant mortality are lower among mothers who have completed at least a high school education in comparison with those who have not completed high school. More educated women are more likely to attain higher income levels and engage in positive health behaviors such as avoidance of smoking during pregnancy. Also, women who have higher income levels usually have more access to health care services than those who have lower incomes.
According to the Office of Minority Health, promising strategies for reducing disparities in infant mortality include encouraging pregnant women to adopt healthful behaviors and lifestyles, to seek prenatal care, and to avoid practices that can affect birth outcomes adversely. For example, interventions might strive to improve pregnant women's nutritional status, increase their access to prenatal care early in pregnancy, and treat their chronic illnesses (CDC, 2012e). Other interventions might include programs for smoking cessation and avoidance of alcohol during pregnancy. As noted previously, cigarette smoking and alcohol consumption increase the risk of adverse birth outcomes.
Causes of Infant Mortality
The 10 leading causes of infant deaths in 2009 are shown in Table 5.1. About 20% of infant deaths were caused by congenital malformations and related conditions. The next highest percentage (about 17%) were associated with disorders related to short gestation and low birth weight. Sudden infant death syndrome caused 8.4% of infant mortality. Maternal complications of pregnancy and unintentional injuries caused 6.1% and 4.5% of infant deaths, respectively. The following sections will cover these five causes in more detail.
| Table 5.1: Number of infant deaths, percentage of total infant deaths, and infant mortality rates for 2009, United States | ||||
| Rank | Cause of death (based on ICD–10, 2004) | Number | Percent of total deaths | Rate |
| . . . | All causes | 26,412 | 100.0 | 639.4 |
| Congenital malformations, deformations, and chromosomal abnormalities | 5,319 | 20.1 | 128.8 | |
| Disorders related to short gestation and low birth weight, not elsewhere classified | 4,538 | 17.2 | 109.9 | |
| Sudden infant death syndrome | 2,226 | 8.4 | 53.9 | |
| Newborn affected by maternal complications of pregnancy | 1,608 | 6.1 | 38.9 | |
| Accidents (unintentional injuries) | 1,181 | 4.5 | 28.6 | |
| Newborn affected by complications of placenta, cord, and membranes | 1,064 | 4.0 | 25.8 | |
| Bacterial sepsis of newborn | 652 | 2.5 | 15.8 | |
| Respiratory distress of newborn | 595 | 2.3 | 14.4 | |
| Diseases of the circulatory system | 581 | 2.2 | 14.1 | |
| 10 | Neonatal hemorrhage | 517 | 2.0 | 12.5 |
| . . . | All other causes | 8,131 | 30.8 | 196.8 |
| Rates are infant deaths per 100,000 live births. | ||||

Design Pics/SuperStock
Down syndrome is one of the congenital malformations leading the causes of infant mortality in the United States.
Congenital Malformations
In 2009, congenital malformations were the leading cause of infant mortality in the nation. A congenital malformation is
[a] physical defect present in a baby at birth but can involve many different parts of the body, including the brain, heart, lungs, liver, bones, and intestinaltract. [A] [c]ongenital malformation can be genetic, it can result from exposure of the fetus to a malforming agent (such as alcohol), or it can be of unknown origin. (MedicineNet.com, 2012)
Among the types of congenital malformations are Down syndrome, heart defects, limb deformities, cleft palate, and neural tube defects. Infectious diseases (e.g., German measles) and environmental exposures can cause congenital malformations. Serious congenital malformations can produce long-term disabilities and devastating impacts upon the affected person, families, and society.
Low Birth Weight
Low birth weight is the term used to describe a birth weight of less than 2,500 grams (about 5.5 pounds) (CDC, 2009). In 2009, low birth weight was among the second leading causes of infant mortality. Low birth weight is a risk factor for several types of health problems including neurodevelopmental disabilities and inspiratory illnesses. Variables associated with low birth weight are described later in the chapter.
Preterm (Premature Births)
The definition of preterm (premature) birth "is the birth of an infant prior to 37 weeks gestation" (CDC, 2012n). Fetuses born before the full gestation period have a greater risk of complications than full-term infants. Slightly more than 12% of births (500,000 births) in the United States are preterm births. They are significant for community health because of their association with infant death and long-term neurological disabilities including cerebral palsy among children. The risk of adverse health outcomes associated with preterm births increases with shorter gestation periods; such outcomes can occur even among infants who are slightly preterm. Another aspect of preterm births is racial and ethnic disparities in their occurrence. The highest rates occur among Black women and the lowest among Asian or Pacific Islander women (Institute of Medicine, 2006).
Sudden Unexpected Infant Death/Sudden Infant Death Syndrome
Sudden unexpected infant deaths (SUIDs) are defined as "deaths in infants less than one year of age that occur suddenly and unexpectedly, and whose cause of death are not immediately obvious prior to investigation" (2012q). Figure 5.3 shows six causes plus a category of unknown causes of SUID in the United States. Sudden infant death syndrome (SIDS) is one of the component causes of SUID and is responsible for about half of cases of SUID. Other causes of SUID shown in the figure include poisoning, suffocation, and infections.
Figure 5.3: Sudden unexpected infant death syndrome (SUID)
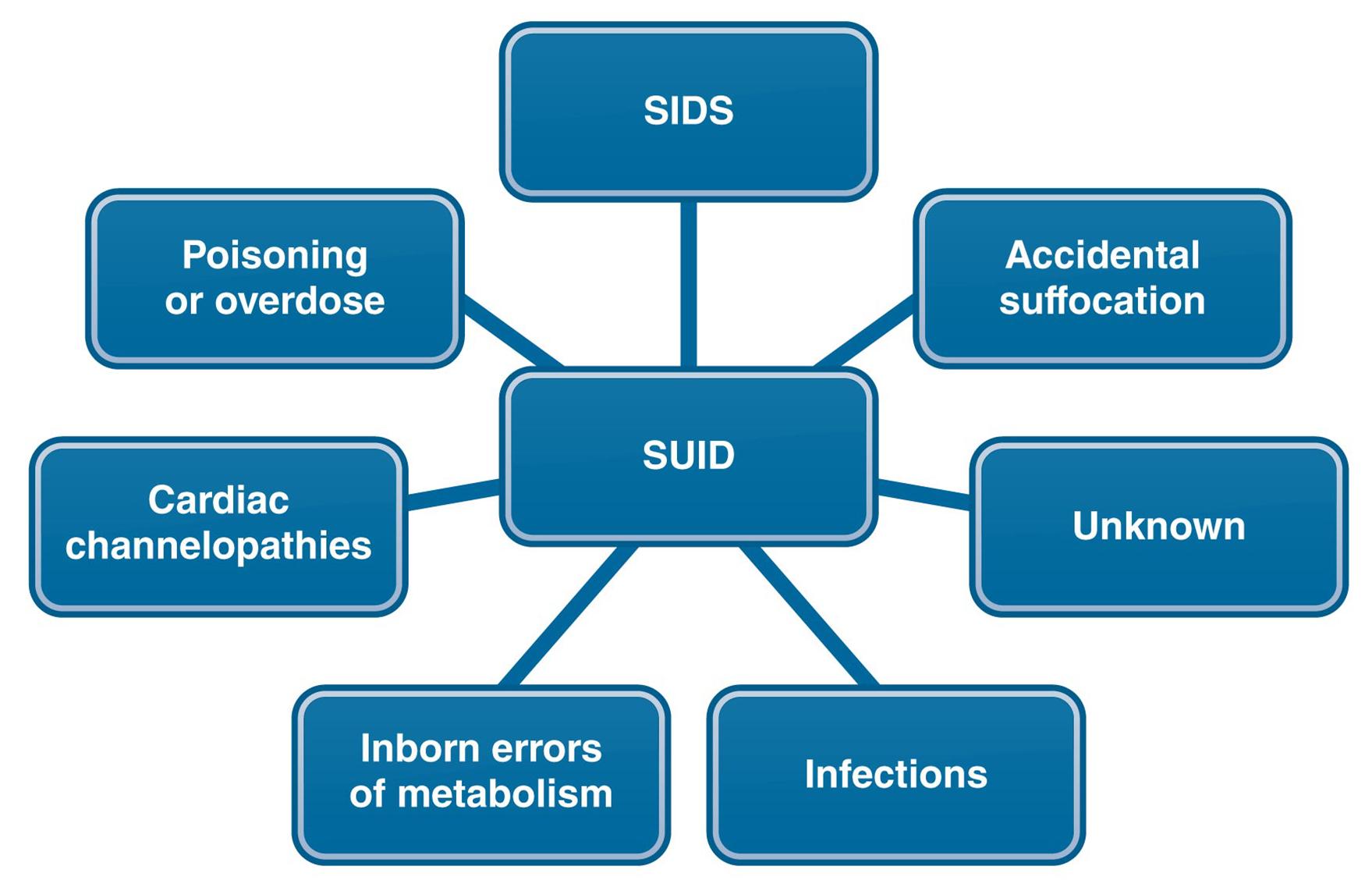
Many of the known causes of SUID can be prevented. How can public health professionals help protect infants?
Sudden infant death syndrome (SIDS) refers to "the sudden death of an infant less than 1 year of age that cannot be explained after a thorough investigation is conducted, including a complete autopsy, examination of the death scene, and review of the clinical history" (CDC, 2012q). Thus, a distinguishing characteristic of a death from SIDS is that no cause can be found even after an autopsy has been performed. SIDS is the third leading cause of infant mortality in the United States.
Maternal Risk Factors for Adverse Birth Outcomes
Healthy mothers tend to produce healthy infants. However, a mother's health, when unsatisfactory, is associated with adverse birth outcomes such as fetal and infant mortality. The mother's health is a determinant of her infant's morbidity, disability, impairments, and congenital malformations. In advance of becoming pregnant, women can improve the health of their infants through maintaining good nutrition, control of chronic diseases, and establishment of a healthy lifestyle that includes avoidance of risk factors for pregnancy complications. Older women have an increased risk of giving birth to an infant with Down syndrome. Other examples of maternal risk factors are provided in Table 5.2.
| Table 5.2: Examples of selected maternal risk factors for adverse birth outcomes | |
| Diabetes | Alcohol consumption |
| Hypertension | Cigarette smoking |
| Heart disease | Sexually transmitted diseases |
| Older maternal age | Prescription and nonprescription drugs |
| Poor maternal nutrition | Infectious diseases |
| Maternal obesity | Exposures to environmental toxins |
Diabetes
A form of diabetes known as gestational diabetes mellitus (GDM) is associated with pregnancy. GDM, an impairment of the body's capability for processing carbohydrates, causes an increase in blood glucose levels. GDM affects from 2% to 10% of pregnant women (CDC, 2012d). In most cases, the condition resolves after delivery, but GDM is associated with the onset of diabetes among some women following pregnancy. Persistently high blood sugar among women with GDM increases the likelihood of preeclampsia, which is characterized by hypertension, protein in urine, and edema. Other outcomes of GDM are preterm births and the need for cesarean births. Pregnant women who have preexisting diabetes (type I or type II) can experience the triggering or exacerbation of health issues including hypertension, heart disease, and blindness. Pregnant diabetic women whose blood sugar continues to be elevated have increased risks of miscarriage, stillbirths, and other adverse birth outcomes.
Hypertension/Cardiovascular Disease
Potential effects of maternal hypertension upon the fetus are infant death, preterm delivery, and small size for gestational age. For the pregnant woman, hypertension is related to risk of maternal complications from preeclampsia and gestational diabetes, and placental abruption (CDC, 2011d). During a normal birth, the baby is born first, and then a few minutes later the placenta separates from the uterus and is expelled from the body; when placental abruption occurs during delivery, the placenta separates from the wall of the uterus before a baby is born. Severe maternal hemorrhaging can result.
Maternal Obesity
As the prevalence of obesity has increased in this country, obesity among pregnant women also has become increasingly common. Obesity during pregnancy occurs among approximately 20% of pregnant women (CDC, 2012m). Obesity increases the risk of several important complications during pregnancy, including:
Gestational diabetes
Hypertension
Preeclampsia
Need for cesarean section.
Alcohol Consumption During Pregnancy
Pregnant women and sexually active women who are not using contraception should not consume alcohol. The CDC states that "there is no known safe amount of alcohol to drink while pregnant. There is also no safe time during pregnancy to drink and no safe kind of alcohol. CDC urges pregnant women not to drink alcohol any time during their pregnancy" (CDC, 2010b). Refer to Health Care in Action: Pregnancy and Alcohol Consumption for the U.S. Surgeon General's statement on alcohol.
Health Care in Action: Pregnancy and Alcohol Consumption
Based on the current, best science available, we now know the following:
Alcohol consumed during pregnancy increases the risk of alcohol-related birth defects, including growth deficiencies, facial abnormalities, central nervous system impairment, behavioral disorders, and impaired intellectual development.
No amount of alcohol consumption can be considered safe during pregnancy.
Alcohol can damage a fetus at any stage of pregnancy. Damage can occur in the earliest weeks of pregnancy, even before a woman knows she is pregnant.
The cognitive deficits and behavioral problems resulting from prenatal alcohol exposure are lifelong.
Alcohol-related birth defects are completely preventable.
Source: CDC. (2005). Advisory on Alcohol Use in Pregnancy. A 2005 message to women from the U.S. Surgeon General. Retrieved from http://www.cdc.gov/ncbddd/fasd/documents/sg-advisory.pdf
Fetal alcohol spectrum disorders (FASDs) are an example of a condition that can affect children born to mothers who consumed alcohol during pregnancy. FASDs cause abnormalities of the face and body structure, low body weight, and behavioral and intellectual deficits.

CARDOSO/BSIP/SuperStock
According to the CDC, no amount of alcohol is safe to drink while pregnant.
Maternal Tobacco Use During Pregnancy
Cigarette smoking during pregnancy increases the risk for a group of severe health problems among fetuses and newborn infants. Among the risks that pregnant women incur when they smoke are lowered fertility, miscarriage, placental abruption, preterm birth, SIDS, certain birth defects (e.g., cleft lip or cleft palate deformity), and infant death (CDC, 2012o). Despite these adverse consequences, about 13% of women in the United States smoke during the last 3 months of pregnancy. In addition to cigarette smoking, a pregnant woman's exposure to secondhand cigarette smoke is also harmful. One of the possible adverse effects of secondhand cigarette exposure is low birth weight.
Sexually Transmitted Infections
Sexually transmitted infections can cause serious consequences for the developing fetus and newborn (CDC, 2011e). Spread of infections from mother to fetus or newborn is called vertical transmission. Among pregnant women, the four most common STIs and their approximate numbers of cases, respectively, are bacterial vaginosis (1,080,000), genital herpes simplex virus 2 (880,000), trichomoniasis (124,000), and chlamydia (100,000). Some of the risks of STIs during pregnancy are infection of the fetus while in utero, transmission of the STI to the newborn during delivery, stillbirths, low birth weight, and neonatal sepsis.
HIV, another STI, can be passed from mother to fetus during pregnancy, from mother to newborn during delivery, and from mother to infant during breastfeeding. Risk factors for vertical transmission of HIV include exposure of the fetus to HIV while in utero and to mother's blood and bodily secretions during birth. Also, breast milk from mothers infected with the HIV virus can transmit the virus to breastfed infants (Buchanan & Cunningham, 2009). At present, the possibility of vertical transmission of HIV is increased among pregnant women who are not tested for HIV. Often, pregnant women are not tested on a timely basis because they do not receive prenatal care.
Infectious Diseases
When a pregnant woman has acquired an infectious disease and this disease crosses the placental barrier to infect the fetus, it is called a congenital infection. The common types of these infections are described by the acronym TORCH (About.com, 2009), which stands for:
Toxoplasmosis
Other infections (e.g., chickenpox)
Rubella
Cytomegalovirus
Herpes simplex virus
For example, chickenpox and rubella (German measles) are vaccine preventable diseases that can cause birth defects when they infect the fetus.
Environmental Toxins
Environmental chemicals and toxins are linked to adverse birth outcomes. Examples of potentially hazardous substances and exposures are prescription and nonprescription drugs, heavy metals (e.g., lead and mercury) present in the residential environment and food, pesticides, industrial chemicals, and ionizing radiation from x-rays and naturally occurring sources. More information on this topic is presented in Chapter 7.
5.4 Children
This section
information on the health status of children in the age ranges of early childhood (1 to 4 years—toddler and preschool ages) and school age (5 to 11 years—middle childhood). According to the CDC, a total of 82.2% of school-age children have excellent or very good health status.

Fancy Collection/SuperStock
Individuals begin to develop the skills they need to live healthfully early in life. The development of healthy habits, like exercise, starts during childhood.
The period of early childhood is important because it is during this time that children develop habits and behaviors that impact their health throughout their lifespan (CDC, 2011c; CDC, 2012f; CDC, 2011b). Desirable lifestyle practices such as consumption of healthful foods, participation in vigorous exercise, and avoidance of substances (tobacco, drugs, and alcohol) are established and reinforced during the school-age years. Much work needs to be done to encourage children to consume a healthy diet, as 20% of school-age children during 2007 and 2008 were obese.
The discourse on the health of children should include the role of fathers in addition to the importance of mothers in promoting the health of children. Fathers who have positive relationships with the mothers of their children are likely to contribute to the development of children who are psychologically healthy, emotionally secure, and who perform well in school (Rosenberg and Wilcox, 2006). Effective fatherhood involves devoting time to children, making sure that their material needs are met, and being a good role model.
The next sections assess trends in child mortality and morbidity. From the international perspective, child mortality continues to be at unacceptably high levels as a result of the impact of malnutrition and infectious diseases. In this country, unintentional injuries are the leading cause of child mortality. Among the most frequent causes of morbidity in America are infectious diseases, asthma, and developmental disabilities.
Mortality Among Children
Stressing the global point of view, WHO indicates that levels of child mortality continue to be unacceptably high, especially in less developed areas. Developed countries have a somewhat more favorable child mortality profile. In the United States, mortality reaches its lowest level among children, and then increases as persons grow older. Child mortality is highly preventable and can be reduced greatly through improvement of environmental conditions and hygiene levels, as well as increased parental compliance with immunizations for vaccine preventable diseases.
International Trends in Child Mortality
The number of deaths among children remains high even though progress in reducing child mortality has been made since 1990. WHO provides worldwide information on the leading causes of death and the percentage of deaths among children younger than 5 years of age. In 2011, globally, there were a total of 6.9 million deaths among children under the age of 5. Many of these deaths were caused by preventable or easily treatable conditions or by malnutrition (WHO, 2012c; WHO, 2012a). The leading causes of death were pneumonia (18%), preterm birth complications (14%), diarrhea (11%), birth asphyxia (9%), malaria (7%), and all other causes (41%). Almost three-quarters of the child deaths happened in Africa and Southeast Asia.
Approximately 20 million of the world's children were afflicted with severe malnutrition in 2010. WHO advocates exclusive breastfeeding of infants as a method for improving the nutritional status of children and preventing childhood diarrhea and respiratory infections.
Leading Causes of Children's Deaths in the United States
With respect to the United States in 2010, Figure 5.4 shows the leading causes of children's death for three age groups of children: 1 through 4, 5 through 9, and 10 through 14. In all three age groups, unintentional injuries were the leading cause of death (CDC, 2012t). Among toddlers, the second most frequent cause of death was congenital anomalies. Cancer was the second leading cause of death among school-age children. The third leading cause of death for school-age children was suicide. Chronic diseases (e.g., heart disease, chronic lower respiratory disease, and cerebrovascular diseases) also were among the leading causes of death for children. Note that the death rate among school-age children was lower than that among children aged 1 to 4 years. Overall statistics regarding mortality among children in 2011 are shown in Table 5.3.
| Table 5.3: Mortality among children in 2011 (United States) | ||||||||
| Age | 1–4 years | 5–14 years | ||||||
| Number of deaths | 4,450 | 5,651 | ||||||
| Deaths per 100,000 population | 26.1 | 13.9 | ||||||
| Leading causes of death |
|
| ||||||
| Source: Centers for Disease Control and Prevention. (2012). FastStats. Child health. Mortality. Retrieved from http://www.cdc.gov/nchs/fastats/children.htm | ||||||||
Figure 5.4: Leading causes of death in 2010 for four age groups: 1–4, 5–9, 10–14, and 15–24
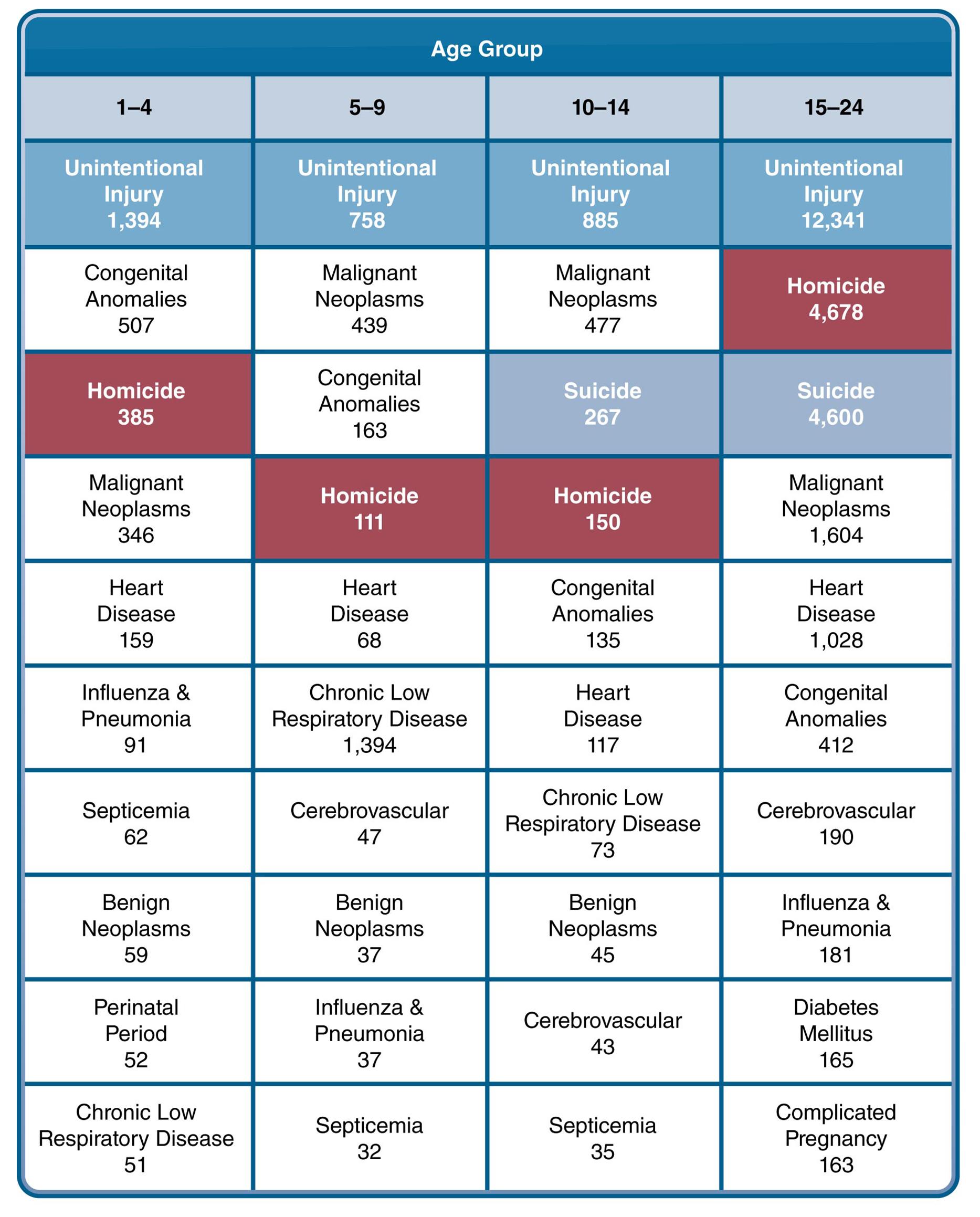
Source: Data adapted from CDC. Retrieved from http://www.cdc.gov/injury/wisqars/leading_causes_death.html
Many public health issues can lead to deaths in younger populations. How can unintentional injuries, homicide, and suicide be prevented in these groups?

National Geographic/SuperStock
The greatest causes of child death throughout the world, such as malnutrition, tend to be preventable.
Morbidity Patterns Among Children
This section covers illness due to a range of conditions: infectious diseases, asthma, and developmental disabilities. Although infectious diseases can occur at any age, some often appear during childhood, when children have not yet developed immunity against them. Also, childhood is a stage of life when developmental disabilities that can last a lifetime begin to appear.
Infectious Diseases and Conditions
Children are susceptible to numerous infectious diseases, which include the common cold and influenza, foodborne illness, diarrheal illnesses, pneumonia, and streptococcal and staphylococcal infections. Chapter 4 presented information on this topic.
One group of infectious diseases, for which vaccines are available, is called vaccine preventable diseases. These are diseases such as hepatitis, diphtheria, polio, influenza, chickenpox, and meningitis. Recommended immunization schedules are somewhat different for children aged 0 to 6 years and 7 through 18 years (CDC, 2012i). Among younger children, the recommended immunization schedule covers 11 diseases (e.g., hepatitis B, rotavirus, and Haemophilus influenzae type b). Recommendations for older children include vaccinations for 10 diseases, including the human papilloma virus (HPV), for which a relatively new vaccination is now available. High levels of children's compliance with recommended immunization schedules are vital to controlling unnecessary outbreaks of infectious diseases and protecting the health of the community.
Asthma
Asthma is one of the most common chronic diseases among children in this country and also a major cause of school absenteeism (CDC, 2012b). The symptoms of asthma include breathing difficulties such as wheezing, chest tightness, and coughing; fatal attacks can occur. Triggers for asthma attacks are tobacco smoke and dust mites.
The prevalence of asthma is on the rise and increased between 2001 and 2009 (CDC, 2011a). During 2007, a total of 185 children's deaths from asthma were reported in the United States. In 2009, the prevalence of asthma among children reached 10%; the condition was more common among boys than girls. The highest rate of childhood asthma (17%) in 2009 was among non-Hispanic Black children, though the reasons for this high rate are not clearly understood yet.
Developmental Disabilities
Developmental disabilities are "a group of conditions due to an impairment in physical, learning, language, or behavior areas" (CDC, 2012c). Often, developmental disabilities become apparent when a child is not meeting age-appropriate developmental milestones—for example, walking or talking. Developmental disabilities usually are permanent and continue throughout a person's life. The causes of developmental disabilities include genetic factors, smoking and drinking during pregnancy, infections during pregnancy, and exposures to environmental toxins. An example of a developmental disability is Down syndrome, which is a chromosomal abnormality. Table 5.4 shows other examples of developmental disabilities. The following sections provide more detail on some of the noteworthy developmental disabilities.
| Table 5.4: Examples of developmental disabilities | |
| Attention-Deficit/Hyperactivity Disorder (ADHD) | Intellectual disability |
| Autism Spectrum Disorders (ASDs) | Kernicterus (brain damage caused by untreated jaundice among newborns) |
| Cerebral palsy (CP) | Muscular dystrophy |
| Fetal alcohol spectrum disorders | Tourette syndrome |
| Fragile X syndrome | Vision impairment |
| Hearing loss | Learning disability |
| Source: CDC. (2012). Developmental disabilities. Specific conditions. Retrieved from http://www.cdc.gov/ncbddd/developmentaldisabilities/specificconditions.html | |
Attention-Deficit/Hyperactivity Disorder (ADHD) is a condition that is marked by difficulty in paying attention and lack of impulse control (CDC, 2010a). ADHD typically begins in childhood and continues into adulthood. Many children normally have difficulty concentrating on a specific task and misbehave from time to time. Eventually, normal children outgrow these behaviors; among children with ADHD, these symptoms persist into older childhood, causing adjustment difficulties. The etiology of ADHD remains unknown, although there may be a genetic linkage. Some of the symptoms of ADHD are:
Difficulty paying attention in class
Frequent daydreaming
Easily distracted
Keeping in constant motion
Not thinking before acting.
Autism Spectrum Disorders (ASDs) are a group of disorders that involve difficulties in social interaction and impairment of language, thinking, and feelings (National Institute of Environmental Health Sciences [NIEHS], 2012). A 2008 surveillance program of more than 300,000 children aged 8 years reported that the estimated prevalence of ASD was 11.34 per 1,000 children. The prevalence of ASD was higher among boys (18.4 per 1000 boys) than among girls (4.0 per 1000 girls). The condition was more prevalent among non-Hispanic White children than among either non-Hispanic Black children or Hispanic children (CDC, 2012h). The causes of ASD have not been fully elucidated, although some research points to the role of genetic background and interactions between genes and the environment. For example, a study of twins suggested that autism is an inherited disorder influenced by environmental factors (Hallmayer et al., 2011). Twins share genetic characteristics as well as common prenatal and early postnatal environments, suggesting that both genetic and environmental influences are implicated in autism. It is hypothesized that environmental factors play a role in triggering or suppressing genetic susceptibility to autism during crucial developmental stages of life.
Intellectual Disability, also called mental retardation, is characterized by delay in reaching developmental milestones such as sitting up and walking, difficulty in speaking, and impairment of memory (CDC, n.d.). Intellectual disability can range in severity from mild to severe. The potential causes of intellectual disability are injuries, infections, and diseases that affect the brain, Down syndrome, genetic conditions, and birth defects. According to data from the National Health Interview Survey for 1997 through 2008, the prevalence of intellectual disabilities is 0.71% (0.59% among children ages 3 through 10 and 0.84% among children ages 11 through 17). The condition is more prevalent among non-Hispanic Blacks, boys, children of mothers who have lower educational levels, and children from families who are below 200% of poverty level (Boyle et al., 2011).
5.5 Adolescents
Adolescence, a time of life when children initiate the transition into adulthood, has noteworthy patterns of morbidity and mortality, many of which are a reflection of lifestyle and behavior. Patterns observed in late adolescence predict many of those that occur among young adults. Consequently, mortality and morbidity data for older adolescents and young adults often are combined for statistical purposes. Chapter 6 will extend the coverage of the material presented on adolescent health in this section.
Healthy People 2020 prioritizes adolescent health, which is crucial for one's entire life. The goal of Healthy People with respect to this topic is to "[i]mprove the healthy development, health, safety, and well-being of young adolescents and young adults" (HealthyPeople.gov, 2012a, para. 1). Health-related behaviors that are established during adolescence tend to carry over into adulthood and affect individuals later in life. Health Care in Action: Healthy People 2020 Summary of Objectives provides the summary of Healthy People 2020's objectives in the domain of adolescent health.
Health Care in Action: Healthy People 2020 Summary of Objectives
Adolescent Health
Number and Objective Short Title
AH–1 Adolescent wellness checkup
AH–2 Afterschool activities
AH–3 Adolescent-adult connection
AH–4 Transition to self-sufficiency from foster care
AH–5 Educational achievement
AH–6 School breakfast program
AH–7 Illegal drugs on school property
AH–8 Student safety at school as perceived by parents
AH–9 Student harassment related to sexual orientation and gender identity
AH–10 Serious violent incidents in public schools
AH–11 Youth perpetration of, and victimization by, crimes
Source: HealthyPeople.gov. (n.d.). Healthy People 2020 summary of objectives. Adolescent health, p. AH-1. Retrieved from http://www.HealthyPeople.gov/2020/topicsobjectives2020/pdfs/HP2020objectives.pdf

Blue Jean Images/SuperStock
As teenagers begin to make their way into adulthood, their patterns of behavior change too. These new lifestyle behaviors affect adolescent mortality rates.
Causes of Death Among Adolescents
During both late and early adolescence, the leading cause of death is unintentional injuries. The other leading causes of mortality vary somewhat between younger adolescents and older adolescents, whose mortality patterns are similar to those of young adults. (Refer to Figure 5.4.)
In 2010, the three leading causes of death among 10- to 14-year-old children were unintentional injuries, malignant neoplasms, and suicide (CDC, 2012t). Other major causes were homicide, congenital anomalies, chronic lower respiratory disease, benign neoplasms, heart disease, cerebrovascular diseases, and septicemia. Among 15- to 24-year-olds, the three leading causes of death in 2010 also were unintentional injuries and suicide (rank 1 and 3), with homicide ranked in second place. Many of the remaining causes of death for this age group were similar to the patterns observed among 10- to 14-year-olds with the exception of the addition of malignant neoplasms, influenza and pneumonia, and complications of pregnancy. Septicemia, benign neoplasms, and chronic lower respiratory disease did not rank among the 10 leading causes for the older age group.
Table 5.5 gives 2009 data on the causes of death for older teenagers (15 to 19 years of age) and excludes young adults. Once again the leading cause of death was unintentional injuries. Chronic lower respiratory diseases were among the leading causes of death for older teenagers, as was also true of 10- to 14-year-old children.
| Table 5.5: Leading causes of death all races, both sexes, 15–19 years, 2009 | ||||||
| Rank | Cause of death | Number | Percent of total deaths | Death rate | ||
| . . . | All causes | 11,520 | 100.0 | 53.5 | ||
| Accidents (unintentional injuries) | 4,807 | 41.7 | 22.3 | |||
| Assault (homicide) | 1,919 | 16.7 | 8.9 | |||
| Intentional self-harm (suicide) | 1,669 | 14.5 | 7.7 | |||
| Malignant neoplasms | 644 | 5.6 | 3.0 | |||
| Diseases of heart | 335 | 2.9 | 1.6 | |||
| Congenital malformations, deformations, and chromosomal abnormalities | 230 | 2.0 | 1.1 | |||
| Influenza and pneumonia | 163 | 1.4 | 0.8 | |||
| Chronic lower respiratory diseases | 86 | 0.7 | 0.4 | |||
| Septicemia | 61 | 0.5 | 0.3 | |||
| 10 | Cerebrovascular diseases | 60 | 0.5 | 0.3 | ||
| . . . | All other causes (residual) | 1,546 | 13.4 | 7.2 | ||
| Source: Data from Heron, M. (2012). Deaths: Leading causes for 2009. National Vital Statistics Reports, 61(7), 17. | ||||||
In summary, injuries of all kinds rank among the leading causes of death for teenagers. In addition to injuries, many of the causes of death have behavioral determinants. The remainder of this section presents information on injuries and behaviorally related risk factors for adverse health outcomes.
Injuries: Unintentional and Intentional

Image Source/SuperStock
Car accidents are the leading cause of unintentional injury and death among adolescents.
The CDC defines an injury as "unintentional or intentional damage to the body resulting from acute exposure to thermal, mechanical, electrical, or chemical energy or from the absence of such essentials as heat or oxygen" (CDC, 2010c). As noted, unintentional injuries and intentional injuries (homicide, suicide, and poisoning) are the leading causes of adolescent deaths. Injury-related causes account for about 67% of all deaths among children and adolescents between the ages of 5 and 9 years (CDC, 2010c). Representative statistics from 2005 for injury deaths are as follows:
Motor vehicle injuries—48% of injury deaths
Homicide—16% of injury deaths, varies by race/ethnicity with highest rates among Blacks in comparison with non-Hispanic Whites.
Suicide—16% of injury deaths.
Violence is one of the major causes of injuries. Examples of violence-associated injuries include:
Youth violence at school and in the community
Dating violence—physical and sexual abuse of a dating partner
Violence against lesbian, gay, bisexual, and transgender (LGBT) youth—school-related violence takes the form of verbal harassment, physical harassment, and physical assaults (CDC, 2011f).
Unintentional Injuries
A common term for unintentional injuries is accidents (referring to a chance occurrence), but the use of this term is discouraged because most unintentional injuries are preventable. Figure 5.5 shows the distribution of deaths from unintentional injuries. Note the major contribution of motor vehicle injuries.
Figure 5.5: Deaths due to unintentional injury among adolescents aged 15 to 19 years, 2007
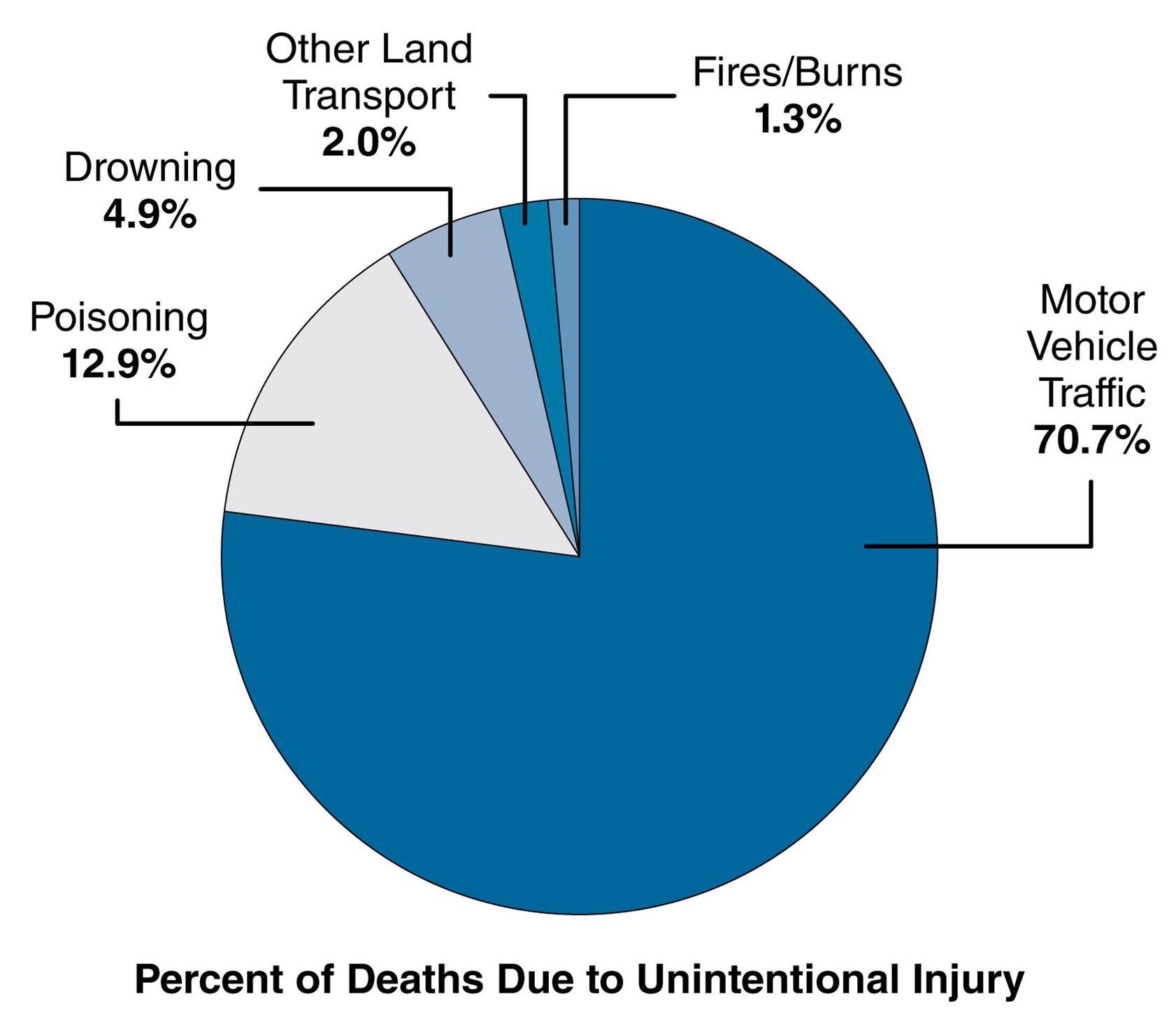
Source: Adapted from Child Health USA. (2011). p. 53. Retrieved from http://mchb.hrsa.gov/chusa11/
Motor vehicle deaths make up over 70% of youth deaths.
Prevention
Each type of injury-related death has a set of identifiable risk factors. For example, failure to wear a bicycle helmet increases the risk of serious injuries from bicycle mishaps. Other examples of risk factors for unintentional injuries and intentional injuries (from suicide and violence) are shown in Table 5.6.
| Table 5.6: Risk factors for unintentional injuries (bicycle- and motor vehicle-related) and intentional injuries (suicide and violence-related) | |||||||
| Unintentional Injuries | Suicide | Violence | |||||
| Rarely or never wore a bicycle helmet | Felt sad or hopeless | Carried a gun or other weapon | |||||
| Rarely or never wore a seat belt | Seriously considered attempting suicide | Carried a weapon on school property | |||||
| Rode with a driver who had been drinking alcohol | Made a suicide plan | Threatened or injured with a weapon on school property | |||||
| Drove when drinking alcohol | Attempted suicide | In a physical fight | |||||
| Texted or emailed while driving | Suicide attempt treated by a nurse or doctor | Bullied on school property or electronically bullied | |||||
| Source: Data from Eaton, D. K., Kann, L., Kinchen, S., Shanklin, S., Flint, K. H., Hawkins, J, . . . Wechsler, H. (2012). Youth risk behavior surveillance—United States, 2011. MMWR 61(4, pp. 4-12). | |||||||
Prevention of injuries can be accomplished through the implementation of appropriate, evidence-based, and readily available interventions. For example, many unintentional injuries connected with motor vehicle use are associated with drinking and driving; school-based interventions can discourage underage alcohol consumption. One of the risk factors for self-inflicted injuries (suicide) is severe depression, which has a high success rate for treatment when intervention is begun early.
Youth violence in America is a major public health issue (Hahn et al., 2007). Intentional injuries caused by homicide and school violence are increasingly notorious problems in America's schools and have been linked to carrying weapons and bringing a gun to school. School violence includes physical bullying and intimidation as well as the more recent phenomenon of cyberbullying. Preventive measures for reducing violence include increasing employment for youth, as well as mobilizing community residents and school officials to discourage violent behavior. In addition, sex education programs for students who are attending schools can help to prevent intimate partner violence.
Universal school-based violence prevention programs are directed toward all students regardless of their level of risk for violence (Hahn et al., 2007). An example of such a program is the Violence Prevention Curriculum for Adolescents, which focuses on the causes of violence and development of skills for resisting violent behavior (Hahn et al., 2007). A second example is the Second Step program—directed toward violence prevention skills development and role playing combined with feedback and reinforcement (Hahn et al., 2007). The Safe Dates Program is a 10-session curriculum for adolescents who are involved in abusive relationships (Hahn et al., 2007).
Risk Behaviors Among Adolescents
Obesity in Childhood
Dr. Barbara Korsch and a team of researchers explain the progression of overweight babies to overweight adults, and the challenges in preventing obesity.
Critical Thinking Question:
How can community and public health professionals make positive changes in childhood obesity rates? What might be the most approachable factor of obesity to target for change?
The Youth Risk Behavior Surveillance System (YRBSS) monitors health risk behaviors that are associated with the primary causes of death and disability among a representative sample of U.S. high school students in public and private schools (Eaton et al., 2012). Examples of risk behaviors are failure to wear a seat belt when riding in a car, drinking, smoking, and not using condoms during sexual intercourse. In addition, the YRBSS collects information of the prevalence of obesity, which is related to chronic diseases such as diabetes. From 1999 to 2011, the prevalence of obesity among school-aged youth increased from 10.6% to 13.0% in 2011. Data from the YRBSS and presented in Table 5.7 show time trends in 15 risk behaviors and obesity between the years 1991 and 2011. In 2011, approximately 40% of high school students had at least one drink of alcohol on at least one day during the 30 days before the survey. Slightly fewer than one-fifth of students reported smoking cigarettes on at least one day. Other prevalent risky behaviors included:
riding with a driver who had been drinking
using marijuana
not using any method to prevent pregnancy during sexual intercourse (among students who were sexually active).
Refer to Table 5.7 for more information on selected risk behaviors and obesity.
| Table 5.7: Trends in the prevalence of selected risk behaviors and obesity for all students (9th through 12th grades), National YRBS: 1991–2011 | ||||||||||
| 1991 | 1993 | 1995 | 1997 | 1999 | 2001 | 2003 | 2005 | 2007 | 2009 | 2011 |
| Rarely or never wore a seat belt (when riding in a car driven by someone else) | ||||||||||
| 25.9 | 19.1 | 21.7 | 19.3 | 16.4 | 14.1 | 18.2 | 10.2 | 11.1 | 9.7 | 7.7 |
| Rode with a driver who had been drinking alcohol one or more times (in a car or other vehicle during the 30 days before the survey) | ||||||||||
| 39.9 | 35.3 | 38.8 | 36.6 | 33.1 | 30.7 | 30.2 | 28.5 | 29.1 | 28.3 | 24.1 |
| Carried a weapon on at least 1 day (for example, a gun, knife, or club during the 30 days before the survey) | ||||||||||
| 26.1 | 22.1 | 20.0 | 18.3 | 17.3 | 17.4 | 17.1 | 18.5 | 18.0 | 17.5 | 16.6 |
| Did not go to school because they felt unsafe at school or on their way to work from school on at least 1 day (during the 30 days before the survey) | ||||||||||
| NA | 4.4 | 4.5 | 4.0 | 5.2 | 6.6 | 5.4 | 6.0 | 5.5 | 5.0 | 5.9 |
| Attempted suicide one or more times (during the 12 months before the survey) | ||||||||||
| 7.3 | 8.6 | 8.7 | 7.7 | 8.3 | 8.8 | 8.5 | 8.4 | 6.9 | 6.3 | 7.8 |
| Smoked cigarettes on at least 1 day (during the 30 days before the survey) | ||||||||||
| 27.5 | 30.5 | 34.8 | 36.4 | 34.8 | 28.5 | 21.9 | 23.0 | 20.0 | 19.5 | 18.1 |
| Had at least one drink of alcohol on at least 1 day (during the 30 days before the survey) | ||||||||||
| 50.8 | 48.0 | 51.6 | 50.8 | 50.0 | 47.1 | 44.9 | 43.3 | 44.7 | 41.8 | 38.7 |
| Used marijuana one or more times (during the 30 days before the survey) | ||||||||||
| 14.7 | 17.7 | 25.3 | 26.2 | 26.7 | 23.9 | 22.4 | 20.2 | 19.7 | 20.8 | 23.1 |
| Ever used methamphetamines one or more times (also called "speed," "crystal," or "ice," during their life) | ||||||||||
| NA | NA | NA | NA | 9.1 | 9.8 | 7.6 | 6.2 | 4.4 | 4.1 | 3.8 |
| Ever had sexual intercourse | ||||||||||
| 54.1 | 53.0 | 53.1 | 48.4 | 49.9 | 45.6 | 46.7 | 46.8 | 47.8 | 46.0 | 47.4 |
| Had sexual intercourse with four or more persons (during their life) | ||||||||||
| 18.7 | 18.7 | 17.8 | 16.0 | 16.2 | 14.2 | 14.4 | 14.3 | 14.9 | 13.8 | 15.3 |
| Used a condom during last sexual intercourse (among students who were currently sexually active) | ||||||||||
| 46.2 | 52.8 | 54.4 | 56.8 | 58.0 | 57.9 | 63.0 | 62.8 | 61.5 | 61.1 | 60.2 |
| Did not use any method to prevent pregnancy during last intercourse (among students who were currently sexually active) | ||||||||||
| 16.5 | 15.3 | 15.8 | 15.3 | 14.9 | 13.3 | 11.3 | 12.7 | 12.2 | 11.9 | 12.9 |
| Attended physical education daily | ||||||||||
| 41.6 | 34.3 | 25.4 | 27.4 | 29.1 | 32.2 | 28.4 | 33.0 | 30.3 | 33.3 | 31.5 |
| Obese | ||||||||||
| NA | NA | NA | NA | 10.6 | 10.5 | 12.0 | 13.0 | 12.8 | 11.8 | 13.0 |
| (Numbers shown are percentages and 95% confidence intervals.) | ||||||||||
Teenage Pregnancy
Teenage pregnancy can have unfortunate impacts upon the physical and social health of the teenaged mother, the father, and the community, which must incur substantial economic costs. One of these adverse outcomes is an increase in school dropout rates among teenage girls who become pregnant. Also, teenage pregnancy causes billions of dollars in direct costs for health care and other expenses related to the care of children born to teenagers. Often, children of teenage mothers have lowered school achievement and increased dropout rates; the sons of teenage mothers have higher frequencies of criminality and incarceration (CDC, 2012a). For example, one review reported that the sons of teenage mothers were more than twice as likely to be confined in prison than sons of women who waited to have children until they were in their early 20s (Hoffman, 2006).
In the United States, the number of births among females between the ages of 15 and 19 years in 2011 was 329,797, which was a birth rate of 31.3 per 1,000 (Hamilton, Martin, & Ventura, 2012). In this age range, the number of births declined by 8% from the previous year (CDC, 2012a). Figure 5.6 shows trends in the birth rates among teenaged women aged 15–19 years between 2000 and 2011. The figure demonstrates that birth rates have declined over time among almost all racial and ethnic groups. An exception is the birth rate among 18- to 19-year-old Asian/Pacific Islanders (CDC, 2012a), which group is not shown in the figure.
Figure 5.6: Birth rates (live births) per 1,000 females aged 15 to 19 years by race and Hispanic ethnicity, 2000–2011
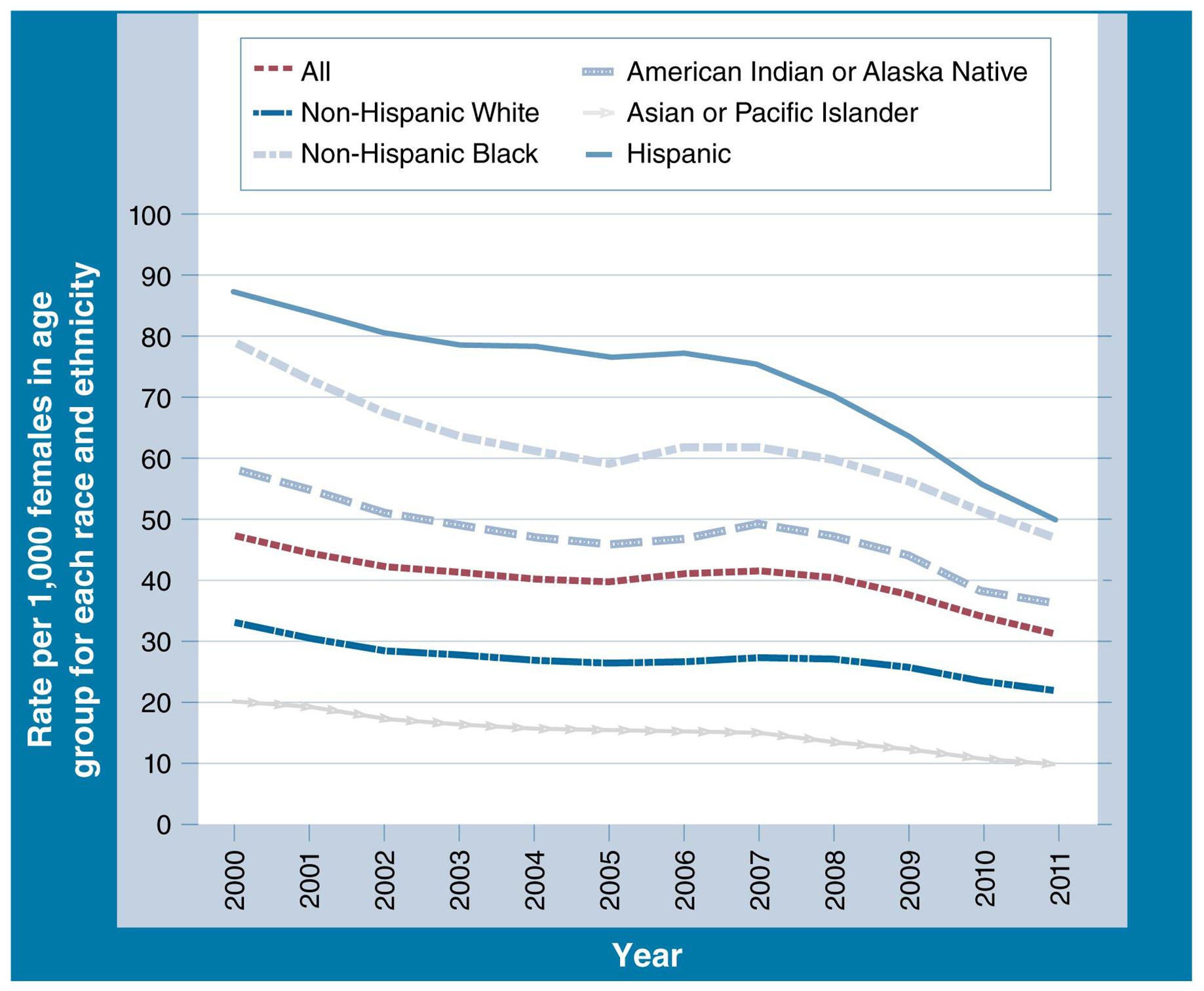
Source: Adapted from CDC.
What does this downward trend in teenage pregnancy and birth suggest about public programs aimed at these populations? What factors might contribute to the disparity between ethnicities?
Racial and Social Disparities in Teenage Birth Rates
Disparities occur among the teenage birth rates of racial and ethnic groups in the United States. The greatest disparities exist among the teenage birth rates of both Hispanic females and non-Hispanic Black females in comparison with other racial and ethnic groups. In 2011, the respective teenage birth rates for Hispanic females and non-Hispanic Black females were 49.4 per 1,000 and 47.4 per 1,000 (Hamilton et al., 2012). Non-Hispanic Black and Hispanic females accounted for about 57% of teen births in 2011 (CDC, 2012a). The rates for non-Hispanic Whites and Asian or Pacific Islanders were 21.8 per 1,000 and 10.2 per 1,000, respectively.
The causes of racial disparities in teenage birth rates are multifactorial. One of the variables associated with lower teenage birth rates is contraceptive use. A larger percentage of sexually active White adolescent females use effective methods of contraception than non-Hispanic Black and Hispanic females (USDHHS, 2013). Another related factor is frequency of sexual activity among different groups. A New York City study reported higher rates of sexual activity among non-Hispanic Black and Hispanic high school girls than among White girls (Waddell et al., 2010). Also, teenage motherhood tends to be transferred across generations, with the daughters of women who were teenagers themselves becoming teenage mothers (Gaudie et al., 2010). Lastly, the risk of teenage pregnancy is higher among families headed by a single parent as well as among dysfunctional families (Gaudie et al., 2010).
Unintended Pregnancies/Abortion
One of the objectives of Healthy People 2020 is to increase the proportion of pregnancies that are intended. About one half of all pregnancies in the United States are unintended, meaning that they are unplanned or unwanted. Among teenagers between the ages of 15 and 17 years, approximately 80% of pregnancies are unintended (CDC, 2012p). Unintended pregnancy is a major contributor to abortion.
According to the CDC, "[A] legal induced abortion is defined as an intervention performed by a licensed clinician (e.g., a physician, nurse-midwife, nurse practitioner, or physician assistant) that is intended to terminate an ongoing pregnancy" (CDC, 2012j). The topic of abortion is subject to much debate. Some of the issues surrounding abortion are whether legal abortions should be permitted at all, the age at which teenagers must have the permission of their parents to obtain an abortion, and the stage of pregnancy (early or late in the pregnancy) during which an abortion may be performed. A more recent concern is the age at which girls may purchase the "Plan B" (morning after) birth control drug. For more information about the controversies surrounding abortion, consult the Planned Parenthood website at http://www.plannedparenthood.org/health-topics/abortion-4260.asp.
Figure 5.7 shows the frequency of abortions in the United States among different age groups. The highest abortion ratio (number of abortions per live births) occurred among females aged 15 and younger. Another measure of the occurrence of abortions is the abortion rate, defined as the number of abortions per 1,000 women (among a particular group of women—for example, a particular age group or racial group) during a year. According to statistics from the CDC, "[i]n 2009, adolescents aged 15–19 years accounted for 15.5% of all abortions and had an abortion rate of 13.0 abortions per 1,000 adolescents aged 15–19 years" (Pazol et al., 2012).
Figure 5.7: Percentage distribution of total abortions, abortion rate, and abortion ratio, by age group of women who obtained a legal abortion, United States (selected states), 2009
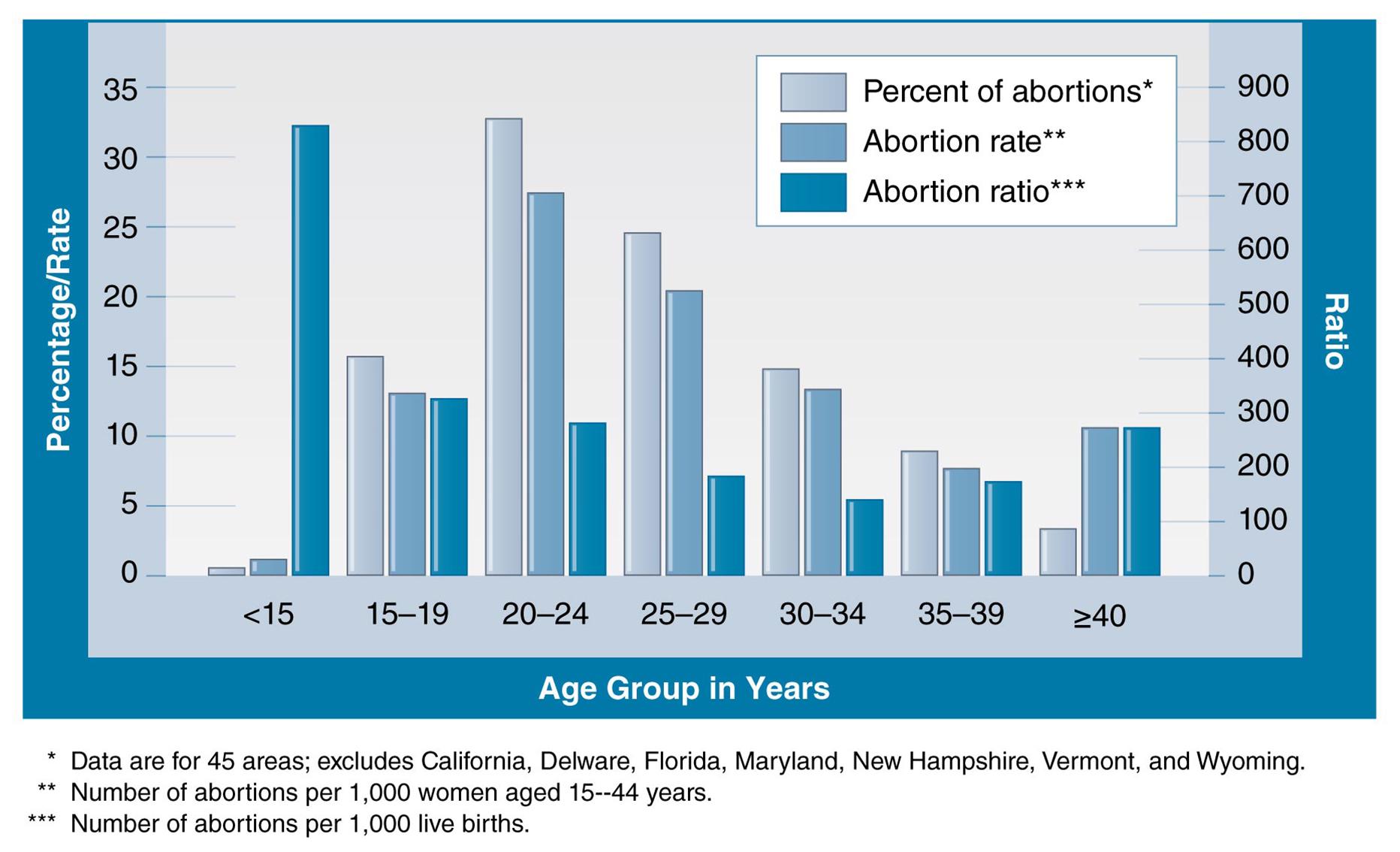
Source: Adapted from CDC, MMWR Abortion Surveillance.
Abortion rates and ratios decrease as a woman ages, while the highest percentages occur in the 20 to 24 age group.
Abortion rates vary substantially across racial and ethnic groups in the United States. In 2009, of three racial/ethnic groups, Black women (classified by the census as non-Hispanic Black women) had the highest abortion rate (42.5 per 1,000 women aged 10 to 44 years) in comparison with Hispanic women (19.3 per 1,000 women aged 10 to 44 years) and non-Hispanic White women (8.5 per 1,000 women aged 10 to 44 years), who had the lowest rate (Pazol et al., 2012). Explanations for the approximately fivefold higher abortion rate among Black women in comparison with non-Hispanic White women are controversial. A likely reason is that Black women have higher rates of unintended pregnancy (Cohen, 2008). As noted, unintended pregnancies (related to low use of effective contraceptive methods) are associated with abortions. Ethical issues in this domain include the fact that some minority women have less access to reproductive health services and birth control methods than non-Hispanic White women.

Karen Kasmauski/Science Faction/SuperStock
Teenagers run the risk of unintended pregnancy by not using methods to prevent pregnancy. Health education programs help to mitigate risk and lower the rate of unintended pregnancy.
Communication between parents and teenagers is one of the central aspects of teenage pregnancy prevention, as is teenagers' access to pregnancy prevention programs. In addition, given the societal costs of teenage pregnancy, the community needs to mobilize in order to prevent this condition. Communitywide initiatives can aid the process of reducing teenage pregnancy by involving all segments of the population. As an example, partnerships can be forged between intervention programs for teenage pregnancy prevention and clinical services based in the community, as well as between schools and clinical settings.
The President's Teen Pregnancy Prevention Initiative lists five components of a teenage pregnancy prevention model, including community mobilization that "supports the sustainability of teen pregnancy prevention programs by empowering community members and groups to take action to facilitate change. This component includes mobilizing necessary resources, disseminating information, generating support, and fostering cooperation across public and private sectors in the community" (CDC, 2012r para. 5). Another component involves working with diverse community partners in order to raise the "awareness of community partners about the link between teen pregnancy and social determinants of health, and ensuring [that] culturally and linguistically appropriate programs and reproductive health care services are available to youth" (CDC, 2012r, para. 9).
While health education programs in schools can be instrumental in disseminating information about risky sexual behaviors in order to prevent teenage pregnancy and reduce the frequency of sexually transmitted infections, studies of the effects of sex education programs for teens have demonstrated contradictory results with respect to their efficacy. Much research has been conducted on this topic; the following are three representative results.
A large national study examined 4,691 male and female teenage and young adult respondents who participated in sex education programs that covered both abstinence and birth control methods. Researchers concluded that individuals who participated in such programs demonstrated healthier sexual behaviors (for example, condom use) in comparison with persons who did not receive such education (Lindberg & Maddow-Simet, 2012).
A program known as "Safer Choices" reduced risky sexual behavior in an HIV-education intervention trial (Kirby et al., 2004). Using an intensive curriculum with several components, the Safer Choices program involved the school environment, staff members, peer groups, parents, and the greater community. Teenaged participants were assigned randomly to either the Safer Choices program or a standard knowledge-based HIV-education program. The intervention demonstrated effectiveness in reducing risky sexual behaviors, particularly among male and Hispanic students and participants who had not used protection against sexually transmitted infections before enrolling in the program and who were at increased risk of conditions such as HIV.
In comparison with the two foregoing examples, other research has not confirmed a positive association between abstinence-only sex education programs and lowered risk of teenage pregnancy and sexually transmitted infections. For example, a study that investigated the impact of four abstinence-only education programs showed that they did not appear to influence various aspects of teenage sexual activity such as knowledge of sexually transmitted infections and perceptions of the effectiveness of birth control methods (Trenholm et al., 2008). The study used an experimental design to compare more than 2,000 teenagers assigned randomly either to one of the four abstinence programs or to a control group.
The evaluation of teenage sex education programs brings us to the final section of this chapter, which concludes with the three core functions of public health: assessment, policy development, and assurance as they apply to maternal, infant, child, and adolescent health.
5.6 Assessment, Policy, and Assurance
This discussion will address the following three questions: How does the community assess the specific needs of the foregoing four groups? What has been done at the public health level to provide population protections (that is, policies and interventions to reduce the occurrence of adverse health outcomes in the population) for these groups? What assurances are there that they are having an impact?
Assessment
Recall from Chapter 1 that one of the core functions of public health departments is assessment, which refers to the ongoing collection and distribution of information about the overall health of the community and needs that exist in the community. Within each community, the assessment function must be relevant to the unique socioeconomic conditions that exist in that particular community in order to impact the most important health needs. The assessment function enables public health departments, policy makers, community members, and other stakeholders to identify priority community health issues and develop strategies for addressing them in an efficient and cost-effective manner. The assessment function is an empirical and science-driven activity. Table 5.8 sets forth examples of data sources and data content and indicates how they may be used for assessment applied to the four population groups covered in this chapter. For example, vital statistics data are collected on a continuing basis by county health departments and states in the United States. One of the types of vital statistics data is birth statistics, which can be used to determine the prevalence of conditions (such as congenital malformations). Similarly, other data sources shown in the table may be used for conducting other types of assessment. Refer to the table for more information about assessments.
| Table 5.8: Public health assessment: Examples of data sources and data content, and their applications to affected populations | |||||
| Examples of Data | Affected Population | ||||
| Data Source | Data Content | Pregnant Women and New Mothers | Infants | Children | Adolescents |
| Vital statistics data collected on a continuing basis | Birth statistics; mortality statistics | Rates of maternal mortality; prevalence of gestational diabetes, hypertension, diabetes | Rates of infant mortality; frequency of congenital malformations | Leading causes of death | Leading causes of death; birth rates among teenagers; death rates for injuries |
| Community screening programs | Participation in screening programs; screening participation rates | Number of women who are screened during pregnancy; frequency of sexually transmitted infections | Infants screened for genetic conditions | Children screened for chronic diseases and obesity | Adolescents screened for sexually transmitted infections |
| Community-based focus groups | Data from questionnaires administered to community members | Women's perceived barriers to receipt of services (e.g., preconception and postnatal care) | Parents' awareness of importance of postnatal care | Parents' awareness of needed immunizations | Adolescents' perceptions of acceptability of health education interventions |
| Descriptive epidemiologic studies that pertain to the community | Epidemiologic analyses of vital statistics data and data from special population surveys | Social and racial distributions of women who do not receive prenatal care | Demographic factors associated with infant mortality; frequency of breastfeeding | Risk factors for childhood mortality | Risk factors for unintentional injuries |
| The Behavioral Risk Factor Surveillance System (BRFSS)—adults and youth | Data on prevalence of behaviors associated with adverse health outcomes | Prevalence of women who smoke during pregnancy | Not applicable | Not applicable | Prevalence of drug use, smoking and alcohol consumption among high school students |
An example of the assessment function of public health was a needs-assessment program operated by the Missouri Department of Health and Senior Services (Missouri Department of Health and Senior Services [MDHSS], 2010). With respect to women's health in the state in 2008, the department found that the rates of several conditions—smoking, obesity, binge drinking, and hypertension—were higher in Missouri than the rates for the rest of the country. Almost half of live births were the result of unintended pregnancies. The death rate for Missouri teenagers in 2006 (53.7 per 100,000) was higher than the national mortality rate (41 per 100,000). Further analysis revealed that this higher mortality rate could be attributed to a higher mortality rate for motor vehicle crashes in comparison with the rest of the nation. As with the assessment conducted in Missouri, once important health priorities have been identified the next step is to develop policies and programs to protect the population from the causes of morbidity and mortality.
Policies for Protecting the Population
The second function of public health departments is to formulate policies that address priority community health issues by using information from assessments that have been conducted. In most instances, public health departments should take the lead in the creation of health policies. An example of a health policy to safeguard the health of the population is prohibiting smoking in restaurants and alcohol-serving establishments in order to prevent exposure of employees and customers to secondhand tobacco smoke. Another possible response for safeguarding community health might be to introduce exercise and dietary interventions for overweight individuals. Finally, in order to prevent motor vehicle crashes, the state department of motor vehicles might restrict the hours when beginning teenage drivers can drive; these restrictions are called graduated licensing. The reader can certainly think of many other public health policies that might be created in order to protect community health.
Consider how policy development can be adapted to the needs of women, infants, and children. Let's distinguish between policies and programs that involve primary prevention (stopping the occurrence of disease) and those that involve secondary prevention (limiting the duration of disease once it has developed). Usually, programs for primary prevention are more cost effective than those for secondary prevention.
Some examples of primary prevention for women and children are the WIC program described earlier, the use of graduated licensing programs for teenagers to prevent car crashes, and school-based sex education programs. Laws that prevent secondhand exposure to cigarette smoke in restaurants and in alcohol-serving establishments are also forms of primary prevention.
Examples of secondary prevention are screening programs for sexually transmitted infections for women before and during pregnancy. Other examples are screening for genetic diseases and for visual problems among schoolchildren. In addition to screening programs, still other examples are programs for persons who abuse alcohol operated by Alcoholic Anonymous and smoking cessation interventions sponsored by the American Lung Association.
The Assurance Function
The assurance function of public health means verifying that priority services identified as part of the assessment and policy-making functions are indeed available to the population and that the services are effective in meeting the needs of the population. Regarding services for women, infants, and children, assurance means confirming that public health agencies offer services needed by these populations. In illustration, the assurance function involves substantiating that prenatal care is available for pregnant women from all income levels in the community and that these women are receiving and utilizing prenatal care. As part of assurance, public health departments are required to verify that infants and children are receiving vital preventive services such as immunizations and health screenings. Finally, public health agencies need to be certain that emergency services are in place to respond to unintentional injuries and motor vehicle crashes that occur among teenagers as well as among all segments of the population.
Another aspect of assurance relates to making sure that public health services and protections are working as intended. Program success can be measured against certain targets for success that have been established. Program effectiveness should also be reflected in the decline in morbidity and mortality rates. For example, during the past 40 years, rates of mortality from coronary heart disease have declined substantially in America, perhaps as a result of public health's increased attention to primary prevention and treatment of heart disease.
An example of the target-setting approach is from Healthy People 2020. The following target for maternal and child health is from Healthy People:
[Maternal Infant and Child Health] MICH–1: Reduce the rate of fetal and infant deaths.
MICH–1.1 Reduce the rate of fetal deaths at 20 or more weeks of gestation.
Target: 5.6 fetal deaths per 1,000 live births and fetal deaths.
Baseline: 6.2 fetal deaths at 20 or more weeks of gestation per 1,000 live births and fetal deaths occurred in 2005.
Target setting method: 10 percent improvement.
Data source [to be used for the outcome assurance]: National Vital Statistics System-Fetal Death and Natality (NVSS–FD, NVSS–N), CDC, NCHS. (HealthyPeople.gov, n.d.)
The foregoing example states that the objective of Healthy People (Objective 1-1) is to reduce the rate of fetal deaths. The target has been set at 5.6 fetal deaths per 1,000, which is below the baseline of 6.2 fetal deaths in 2005. The target setting method is a 10% improvement. Data for assessing outcome will be from the National Vital Statistics System. Similarly, targets for the many other Healthy People 2020 objectives in other health domains have been created.
Healthy People's use of quantitative targets permits a more accurate assessment of successes and failures in reaching goals for maternal, infant, and child health than qualitative impressions. Two illustrations of health outcomes that are assessed are infant mortality and preterm births (before 37 weeks of gestation). For example, with respect to infant deaths, there has been a 5.6% decline (from 7.2 per 1,000 to 6.8 per 1,000) in the nation's infant mortality rates between 1997 and 2007 (HealthyPeople.gov, 2013a). However, the rate plateaued between 2000 and 2007, and ranged from 6.9 per 1,000 to 6.8 per 1,000. The preterm birth rate for the 1997 to 2007 time period increased by 7.6%; this increase was from 11.8% of live births to 12.7% of live births. These successes (reductions) in infant mortality and failures (increases) in preterm births are related to women's access to prenatal care, avoidance of smoking and drinking during pregnancy, and a host of social and economic factors mentioned earlier in this chapter. Results from Healthy People will continue to suggest needed policy changes in order to improve the health of mothers, infants, and children.
Summary
Chapter 5 covered maternal, infant, and child health, including the health of teenagers. The chapter demonstrated that optimizing maternal health was an essential aspect of the health of the community. We also noted that morbidity and mortality vary according to children's life stages.
Significant community health issues during the childbearing years are high levels of infant mortality and mothers' lack of utilization of prenatal health care services. In comparison with many other developed countries, the United States has a high ranking with respect to the country's level of infant mortality. Related to infant health is the phenomenon of adverse birth outcomes associated with lack of prenatal care and risky behaviors such alcohol and tobacco use during pregnancy. Methods for promotion of maternal and child health include family planning, good nutrition, positive lifestyle, breastfeeding during infancy, and provision of childcare to working mothers.
The United States has tended to achieve a high level of children's health, although chronic conditions, preventable diseases, and unintentional injuries are fairly common during childhood. Many of these adverse outcomes could be prevented by encouraging greater adherence to immunizations for vaccine preventable diseases and programs for prevention of unintentional injury avoidance. In addition, parents have become increasingly aware of ADHD and Autism Spectrum Disorders that occur during childhood. Unfortunately, the etiologies of these conditions are not well understood.
During the teenage years, health issues such as teen pregnancy, onset of chronic diseases, and behaviorally linked conditions become salient. The teenage years are a time of increased mortality from chronic diseases such as cancer and heart disease. Other significant health issues for teenagers are unintentional injury deaths and intentional injury deaths that result from interpersonal violence and suicide. Also important for teenagers are conditions associated with risky behaviors including smoking, binge drinking, abuse of prescription and illicit drugs, and unprotected sex.
The chapter concluded with a discussion of assessment, policy development, and assurance as they pertain to the health of mothers, infants, children, and teenagers. Healthy People 2020 provides an excellent example of how assessments are conducted and targets are set for measuring the nation's progress to community health and public health objectives.
Study Questions and Exercises
Discuss the relationship between family planning and positive health outcomes for the family and the community.
Define the term pregnancy-related mortality. What are the three leading causes of pregnancy-related deaths in the United States?
What factors are associated with mortality among infants? Discuss methods for their prevention.
Why is breastfeeding important for the health of infants? In your opinion, what are the influences that discourage breastfeeding in public? How might these barriers be overcome?
Why does the CDC urge pregnant women not to consume alcohol? Is it safe for pregnant women to consume alcohol in small amounts in social settings as long as consumption takes place in moderation? Define the term fetal alcohol spectrum disorders. What are the characteristics of these disorders?
Describe the consequences of smoking among pregnant women for the health of the fetus and newborn infants. What birth defects have been attributed to smoking during pregnancy?
Describe trends in preterm births over time. What adverse health consequences are associated with preterm births? Discuss the variation in preterm birth rates among different racial and ethnic groups in the United States.
Why are teenagers at higher risk of unintended pregnancy than other age groups? What are some methods for preventing unintended pregnancy among teenagers?
Compare and contrast three leading causes of death among children and teenagers. Give explanations for any observed differences.
Describe three risk-taking behaviors that are taken by many teenagers in the United States. Using your own ideas, describe possible community interventions for reducing these behaviors.
Key Terms
Click on each key term to see the definition.
abortion rate
adolescence
Attention Deficit/Hyperactivity Disorder (ADHD)
Autism Spectrum Disorders (ASDs)
cesarean delivery (c-section)
congenital infection
congenital malformations
developmental disabilities
family planning
infant mortality
injury
maternal health
nonmedically indicated
placental abruption
postpartum care
postpartum depression
pregnancy-related death
prenatal care
preterm (premature) births
risk behaviors
sudden infant death syndrome (SIDS)
sudden unexpected infant deaths (SUIDs)
teenage pregnancy
teratogen
Women, Infants, and Children (WIC)



