Health Information Systems and the Electronic Health Record

Neehr Perfect Level I Scavenger Hunt: EHR Orientation
Overview
This Level I Scavenger Hunt is an orientation to Neehr Perfect. This activity provides a detailed overview of the Neehr Perfect EHR and should be completed prior to any other Neehr Perfect activities.
Prerequisites
Read the Student Guide to Neehr Perfect that came with your Program Key. The guide is also found under Help > Guides on www.neehrperfect.com.
Create your Neehr Perfect account and activate your subscription if you haven’t done so already.
Log into Neehr Perfect at www.neehrperfect.com using the username and password you created when activating your account.
Locate the videos under the Help tab and view the Student Orientation video.
Become familiar with other resources in the Help tab.
Student instructions
If you have questions about this activity, please contact your instructor for assistance.
Document your answers directly on this document as you complete the activity. When you are finished, save this document and upload it to your Learning Management System (LMS). If you have any questions about submitting your work to your LMS, please contact your instructor.
Screen displays are provided as a guide and some data (e.g. dates and times) may vary.
Additional resources
Drug Information Portal (National Library of Medicine)
Health Information (Medline Plus)
Lab Tests Online
Links to these resources are found within the EHR and can be used for quick reference or to look up the details of a diagnosis, medication or lab test.
Objectives
Understand what an EHR is, including the various features and functions found in an EHR.
Demonstrate the technical skills necessary to access an EHR system and trouble-shoot and resolve access difficulties.
Locate patient name and open correct record using patient lookup.
Navigate essential areas of a patient electronic medical chart.
Understand how to set personal preferences in an EHR.
Demonstrate how to access and use reference tools and materials associated with an EHR.
Complete documentation in an EHR.
Glossary
EHR: An Electronic Health Record (EHR) is an electronic version of a patient’s medical history. It is maintained by health professionals for a hospital, clinic or a medical provider’s office. It is maintained over time and includes medically relevant data for a person, including demographics, progress notes, problems, medications, vital signs, past medical history, immunizations, laboratory data and radiology reports. The EHR automates access to information and has the potential to streamline the clinician's workflow. The EHR also has the ability to support other care-related activities directly or indirectly through various interfaces, including evidence-based decision support, quality management, and outcomes reporting. These features of an EHR have the potential to help health professionals improve patient care by reducing medical errors and controlling healthcare costs.
The Neehr Perfect EHR is an educational version of the VistA EHR used worldwide in Veteran Administration (VA) hospitals and clinics. VistA is one of the most widely used EHR systems in the world.
Problem: Medical diagnosis or health condition that is identified and placed in the patient’s medical record. A problem can be occurring right now (active), it can be new (acute), it can be something that has been going on for a while (chronic), or it could not even be a concern anymore (resolved). For example: hypertension, pain in left foot, sinus infection, or left femur fracture.
Allergy: A hypersensitivity caused by exposure to a particular antigen (allergen,) resulting in a marked increase in reactivity to that antigen when exposed to it again. Sometimes repeat exposure results in harmful immunologic consequences. Two examples of allergies include: 1) Eating a certain food and breaking out in a rash around the lips. 2) Taking a medication and then not being able to breath.
Postings: Postings contain critical patient-related information about which healthcare professionals need to be aware. The Postings button is visible on all tabs of the EHR and is always located in the upper right corner of the window. Postings are also displayed in a window on the Cover Sheet. Specific notes can be designed as postings so that when they are signed on the Notes tab of the chart it will also show on the Cover Sheet. For example, the Lab Results Note V2 can also be seen on the Notes tab.
Vitals: Vitals include heart rate, breathing rate, temperature, blood pressure and rating of pain. Many include the pulse oximetry (measuring oxygen saturation), weight and height when taking vital signs.
BMI: BMI is “body mass index”. This is a person's weight in kilograms (kg) divided by his or her height.
Clinical Reminder: Reminders that assist clinical decision making and also improve documentation and follow-up, by displaying specific tests and evaluations that are due for the patient based on the patient’s age, vital signs, medical problems and documentation in specifically designed notes.
Orders: A formal instruction or request usually authored and entered into the patient’s record by a licensed provider, such as a physician, nurse practitioner, or physician assistant. There are instances when a nurse, medical assistant or HUC (Hospital Unit Coordinator) is granted permission to enter orders on behalf of a provider. These are called transcribed orders and are usually described as ‘verbal orders’ or ‘telephone orders.’ An order is written to direct the care of a patient. It could be for a test to perform, medication to give, an assessment to complete, or care to keep the patient safe.
Discharge Summary: A detailed summary of a patient’s hospitalization. It includes a plan of care for the patient for after discharge: who will care for the patient, referrals, needed equipment, medications, and so on.
Laboratory (Lab) tests: are medical procedures that involve testing samples of blood, urine, or other tissues or substances in the body. Lab tests are used to help determine what is going on with the patient, why the person is sick, and to diagnose the patient. Lab tests can be ordered as an individual test, or as a group, called a panel. The default view in Neehr Perfect is the most recent lab test.
The activity
Go to www.neehrperfect.com and sign in to the Neehr Perfect EHR using your username and password in the login section. The username and password are yours to protect. Do not share them. Follow the HIPAA Privacy Rule and your program’s policy on student conduct when in the EHR.

Select the Start Neehr Perfect EHR button.

Select the EHR icon and enter your username and password (you may be prompted to download the Citrix plug-in if you haven’t done so already). Contact the 24/7 Help Desk if you need assistance. Note: your EHR icon may be named differently than in the image below (i.e. EST01 or PST01).

Once the EHR launches, the Patient Selection window will appear. Search for the patient Frank Stratten by starting to type the last name of the patient – Stratten. The middle name of the patient chart will include the name of your school or program. Double click on the patient name or, once the patient name is highlighted/selected, click OK to open the patient record. Please note: your view in the EHR may vary slightly from the screen shots below.

Cursor actions used in the EHR
Each type of EHR system will have a unique appearance and design, but all EHRs have universal EHR functions. Becoming comfortable accessing the EHR functions is an important part of healthcare training and preparation. In the VistA EHR system, the patient chart is called the computerized patient record system (or CPRS) and it has a simple interface to provide access to the EHR functions. In CPRS, the universal EHR functions can be accessed with a few simple mouse actions.
The single left-click, which allows you to open menus or select data.
The hover, click, hold and drag which allows you to resize areas and move windows on a tab.
The double left-click, which allows you to view details and to open reports.
The right-click, which allows you to access item actions.
To resize windows
Place the mouse cursor on the lines between the boxes, or the sections, on the cover sheet. When the cursor changes to a double arrow (the blue arrows in the above screenshot) click and drag to make the boxes bigger or smaller.
Font size
The default font size for all new user accounts is 8 point. If you are accessing the EHR on a laptop or desktop computer, you may want to enlarge the font.
Edit menu > Preferences > Fonts: Changing font size to 12 or 14 is recommended for desktops, PCs and Macs. An 8 point font is recommended for handheld devices and tablets. Note: After changing the font size, you may need to adjust the layout of your Cover Sheet windows so that all sections are visible.
Date ranges
Date ranges are a filter setting to allow you to view data within a specified time frame. The default setting in the EHR is two days. Change this so that historical data can easily be seen.
Tools menu > Options > General tab and select Date Range Defaults: Change the inpatient and outpatient lab days to 999. Change Appointments and Visits Start date to Today – 999 and the Stop date as Today + 90. Select OK to close the ‘Date Range Defaults on Cover Sheet’ window.

While still in Options, change one more default setting. Click on the Reports tab and select Set All Reports. Changing this personal setting will allow you to view items on the Reports tab of a patient chart without changing the search settings every time. Change the Start Date to 01/01/2010, leave the Stop Date at today’s date (the default date), and change the Max to 999.

Click OK and then Yes when the confirmation box appears. Then click OK again to close the Options window.
External resources available through the EHR
Tools menu > select Drug Information Portal. This will take you out of the EHR and into another window of your web browser. You are now on the webpage supported by the U.S. National Library of Medicine. To get back into the EHR, select the CPRS icon at the bottom of your screen ( or
). Select the Tools menu again, and this time click on Health Information. Again, you will be taken to another Internet browser and the website for Medline Plus. Return to EHR window and repeat the previous steps. Click on Lab Tests Online. This will take you to the website Lab Tests Online.
Help menu
This help menu comes with the CPRS EHR and contains just about anything you might need to know on how to access something specific and help on a topic inside the patient EHR.
Help menu > Contents: You are now in the CPRS Help File. The ‘Find’ or ‘Index’ buttons allow you to search for a variety of help topics. Note: There are additional resources and help options available in the Student Resource Network portion of Neehr Perfect website.
The Cover Sheet tab
The Cover Sheet is time sensitive, showing the most current information that has been entered into the patient chart. Think of it as a snapshot of what is going on with the patient, or the last time documentation was placed in the chart.

Click on the upper left box with the patient’s name, social security number and date of birth. This will open the Patient Inquiry window.
What is the Health Insurance Information listed for this patient?
Blue Cross Blue Shield
Aetna
Affordable Care Act
There is none listed
What is patient’s address?
808 Blue Leaf Lane Minneapolis MN
789 Winding River Road Duluth MN
617 Crest Circle Duluth MN
1412 Winding River Bend Duluth MN
Who is the emergency contact?
Lucille Smith
Lucille Stratten
Lucille Sizemore
There is none listed
Close the Patient Inquiry window by clicking on the Close button. You are now viewing the Cover Sheet again. Locate the Active Problems box in the upper left corner on the Cover Sheet. Click on any Problem.
Which of the following fields are included in the problem’s details?
Onset and Status
Past medical history
Referring provider
Treatment plan
What is the Clinic listed for the problem?
Outpatient Clinic
Emergency Room
Family Clinic
Women’s Health
Close the Problem window by clicking on the Close button. Locate the Allergies/Adverse Reactions box on the Cover Sheet. Click on the patient’s Penicillin allergy. This will give you information about the patient’s reaction to the allergen.
When this patient has a reaction to penicillin, what are the signs and symptoms?
Itching
Hives and watering eyes
Rash
Itching and watering eyes
What is the nature of the reaction?
Pharmacological
Adverse reaction
Sensitivity
Unknown
Close the allergy window by clicking on the X. Click on the Aspirin allergy.
What drug classes are listed for the aspirin allergy?
Antibiotic
Salicylates, Antirheumatic
Anticoagulant, Anti-inflammatory
Sulfonamide
Postings
If a patient record contains postings, the Postings button displays one or more of the following letters: C, W, A, D. These letters correspond to the four types of postings described below.
C (Crisis Notes) – Cautionary information about critical behavior or patient health.
W (Warnings) – Notifications that inform medical center staff about possible risks associated with patients.
A (Adverse Reactions/Allergies) – Posting that displays information about medications, foods, and other items to which patients are allergic or to which they may have an adverse reaction.
D (Directives) – Also called advanced directives, directives are recorded agreements that a patient and/or family have made with the clinical staff.
Locate the Postings window on the Cover Sheet. There are multiple postings in this patient chart. One of the notes listed in the Postings is an Informed Consent. A single click on the posting title, Informed Consent (Electronic), will pull up the contents of the note.
What surgery or procedure is the Informed Consent for?
Appendectomy
Lumbar Laminectomy
Tonsillectomy
Lumbar Stenosis
Close the note window by clicking on the Close button. Close the Postings window by clicking on the Close button. Locate the Vitals window on the Cover Sheet. Here is a list of the abbreviations:
T = Temperature
P = Pulse, or Heart Rate
R = Respirations, or breathing rate
BP = Blood Pressure
HT = Height
WT = Weight
PN = Pain
POX = Pulse oximetry, or oxygen saturation
BMI = Body Mass Index
Click on the temperature (T) entry in the Vitals window. You are brought to the Vitals history of the patient, called Vitals Lite. On the left side panel you can choose the date range of the vital signs you want to view in a graph. Scroll down and choose All Results. Clicking on the horizontal scroll bar will display the details of all of the vitals in the chart.
Notice that Vital Signs can be entered by clicking on the upper right icon Enter Vitals. DO NOT ENTER VITAL SIGNS INTO THIS CHART AT THIS TIME
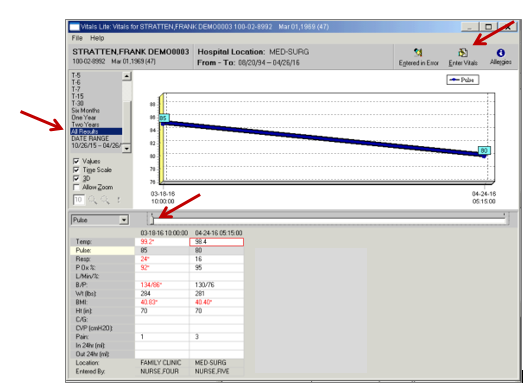
Any vitals that are in red are out of the normal expected ranges for the average adult. These are considered abnormal.
Which blood pressure recorded in this patient’s chart is abnormal?
134/86
130/76
40.40
98.4
When the patient is at Med-Surg, Nurse Five recorded his pain level. On a scale of 1-10, what did the patient rate his pain?
Close the Vitals window to return to the Cover Sheet by clicking on the X.
To locate the patient’s BMI, look in the Vitals window on the Cover Sheet. Hint: Depending on your font size and the adjustment of the windows on the Cover Sheet you may need to scroll down.
What is this patient’s BMI?
40.40
41.44
42.04
43.11
Locate the Clinical Reminders window on the Cover Sheet.
What is the name of the Clinical Reminder related to the patient’s BMI?
Body Mass Index >25 (and/or NP BMI >25)
Body Mass Index <25 (and/or NP BMI <25)
Body Mass Index Abnormal
Body Mass Index Elevated
A single left click on a Clinical Reminder will provide you with information on the clinical maintenance. Right-clicking on the Clinical Reminder will give you the option of looking at the reference information provided for this clinical reminder. Try it! See what information is given for each reminder.
Appointment/Visit/Admission
In the EHR, an appointment or a visit can refer to a time that the patient met with a doctor or specialist at a clinic. For example: a routine appointment, a physical therapy session or a consult with a nutritionist. Appointments and visits are what constitute an “encounter.” These are typically short in time and are considered “outpatient.” An admission is when a patient is admitted to a hospital for an inpatient stay, surgery, or ambulatory procedure. An admission can be for a few hours, a few days, or indefinitely, like with a long term care rehab facility. An admission is considered an “inpatient stay.”
In the Neehr Perfect EHR, each chart can hold information for both inpatient and outpatient events. With this orientation chart, you will see that the patient has two outpatient visits at the Family Clinic and one inpatient stay (hospital admission to the Med-Surg unit). When you opened the chart to begin this orientation, by default the EHR was set to open with the most current event for this patient, which is his current inpatient stay.
The Problems tab
Click on the Problems tab. The problems list on the Problems tab displays a patient’s current and historical health care problems. The problems list allows each identified problem to be traced through the EHR.
Clicking on any of the View Options (Active, Inactive, Both active and inactive, and Removed) will allow you to see what problems are listed under each. New problems can also be added by clicking on New Problem. Double clicking on a problem will display details of the entry. Try it! See what problems are listed under each category listing. Double click on one of the problems to see the details. DO NOT ENTER PROBLEMS INTO THE CHART AT THIS TIME.

What is the patient’s inactive problem?
Wheezing
Low back pain
Spinal stenosis, lumbosacral region
Acute upper respiratory infection, unspecified
The Meds tab
Click on the Meds tab. When you select the Meds tab, you see a list of medications that have been ordered for this patient. If you would like to view additional information about a medication, double click the medication entry or select a medication and choose View > Details. Note: You can also review or add medication orders from the Orders tab. If a medication is preceded by an asterisk (*), the asterisk indicates that the order was changed.
Medications showing on this tab indicate that the medication is active and current for this patient. Remember that Neehr Perfect is an educational EHR. By default, if a medication is more than 100 days old, it is “expired” and will not show on this tab. If there are no medications listed on the Meds tab, then the medication orders are more than 100 days old and have expired. Go to the Orders tab to see any medication orders. In practice, medications may be ordered to be given “one time”, for “24 hours”, or “until discharge.” To view the patient’s medications, both current and expired, go to the Orders tab.
The Orders tab
Click on the Orders tab. When you select the Orders tab, you see a list of orders for this patient. If you would like to view additional information about an order, double click the order entry or select an order and choose View > Details.
Everything is tracked in the EHR and your actions in the EHR leave a digital footprint, including who enters an order in a patient record. In some systems, the EHR will list who entered the order, or who authored it, or list the electronic signature of the person who was signed in with their username and password.
Scroll down until you locate the order for vital signs, “Vital signs per protocol.” Double click on the order.
This is the Order Details.

Whose electronic signature (Elec Signature) is listed for this order?
Nurse One
Nurse Twelve
Doctor Twelve
Doctor Nine
Close the Order Details window. This time perform a single-click to highlight the order, then right-click. Notice all of the options, or “actions” that you have when working with an order.
What is the first option listed?
Details
Results
Renew
Sign
Click on the first option. What are you seeing in the pop-up window?
Information about all of the orders.
Detailed information for just this order.
Instructions to call the doctor.
Nothing, the screen in blank.
Close the window by clicking on the Close button. Click on the Action menu at the top of the chart. Again, notice all of the options that are available to the user.
The Notes tab
Click on the Notes tab. When you select the Notes tab, you see a list of notes for this patient. It provides a central location for current and past information about the patient’s health. This is also where the user is able to document in notes and enter Encounter information.
Notes are used to document information about the patient’s health condition, treatments, test results, communication with the patient, etc. Notes can be used to:
Document in common formats (SOAP, History and Physical, Health History…).
Share data with other members of the healthcare team.
Document patient care and update patient status.
Document something that doesn’t have a specific place holder anywhere else in the chart.
Expand on or explain information.
Provide a comprehensive narrative about the patient’s health.
On the left of the screen is a summarized listing of the notes in the patient chart as determined by your “View” selection (from the View menu option). In the image below, the Last 100 Signed Notes are available to view.

Click on the note titled MED: HEALTH HISTORY (MEDICAL OFFICE). Read the note. You may have to scroll down to see the entire contents. Answer the following questions.
What is the patient’s chief complaint?
“I’m not feeling well.”
“I’m having trouble breathing.”
“I drink alcohol daily.”
“I need to see the doctor.”
The patient had labs drawn. His glucose level was:
9.8
50
108
226
Go to the note titled, LAB RESULTS NOTE V2.
These are the patient’s pre-op labs. What is the patient’s potassium result?
138
25
4.0
Go back to the Cover Sheet. In the Postings window, click on the title Lab Results Note V2. Notice that this is the same note that is on the Notes tab. The Postings box on the Cover Sheet gives you a “quick view” of alerts and important notes that need to be seen quickly, or are important to the patient’s care. Close the Lab Results Note V2 box by clicking on Close.
The Consults tab
Click on the Consults tab.
Consults are requests from one clinician to a hospital, service or specialty for a procedure or other service. A consult can be requested by a medical doctor, a pharmacist, a physical therapist or a licensed professional who has the experience and training to explore a patient’s problems and concerns. A written consult will often have recommendations for treatment included. In Neehr Perfect you may find consults listed on the Consults tab OR on the Notes tab.
The Surgery tab
Click on the Surgery tab.
For the Neehr Perfect EHR, the Surgery tab is not activated. In practice, this tab would be used to coordinate surgical procedures for patients. You will not see any patient surgical information on this tab. Surgical notes, operative notes and anesthesia notes will be found on the Notes tab.
The Discharge Summary tab
Click on the Discharge Summary tab. Authorized health professionals can write, review, edit, save, and sign discharge summaries for individual patients when being discharged, or released, from an inpatient stay or hospitalization.
Not every chart in Neehr Perfect will have a discharge summary. If a patient is still an inpatient in the hospital there won’t be a discharge summary. If the chart is an outpatient chart for a clinic, therapy center or doctor’s office, there may not be a discharge summary. If a chart has a discharge summary written by a provider it will be located on this tab.
Mr. Stratten does not have a discharge summary in his chart. Why?
He has been transferred to another hospital.
He has not been discharged yet.
The information is not available.
He is still at the outpatient Family Clinic.
The Labs tab
Click on the Labs tab. Through CPRS, you can review lab test results in many formats, such as the following: Most Recent, Cumulative, All Tests by (specified) Date, Selected Tests by Date, Worksheet, Graph, Microbiology, Anatomic Pathology, Blood Bank, Lab Status.
What is the most recent lab test showing on the Labs tab?
Red blood cell
Hemoglobin A1c
Glucose POC
There is not a lab test listed.
Go back to the Cover Sheet. In the Recent Lab Results window, click on the lab Glucose Poc Blood. Notice that this is the same lab and result that is on the Labs tab. The Recent Lab Results window on the Cover Sheet gives you a “quick view” of labs that are listed on the Labs tab. Close the Glucose POC Blood box.
The Reports tab
Click on the Reports tab. CPRS reports include Clinical Reports, Health Summary, Imaging (Radiology and Nuclear Medicine), Lab Status, Blood Bank Report, Anatomic Pathology Report, Dietetics Profile, Nutritional Assessment, and Vital Cumulatives. You will see these reports in the Available Reports box.
The Reports tab in the patient chart is a central location to generate just patient healthcare data reports based on the content entered in the patient’s chart. Patient health information can easily be printed from the Reports tab. A report can be something as short and simple as the patient’s demographic information, or long and detailed including all of the orders entered in the patient’s chart. Reports can be sorted by type and dates.
Click on the plus sign (+) next to Clinical Reports. Then click on the plus sign next to Orders. Next, click on Orders Current. Then, on the bottom left side of the screen, under “Date Range,” click on the last option, which will begin with T (for example, T-2442 to T. The number may vary). HINT: If you don’t see this option, refer back to pages 5-6 and ensure you followed the steps to set your date range preferences. You should see orders on the right side of the screen. To better view the orders, place your cursor on the vertical line. Once you have a double arrow you can move the column width. You can also scroll down the list to view all of the orders.

From the Orders Current view locate the following order and finish the order. “Turn, cough and ____________________.”
“…deep breath.”
“…deep breath every hour.”
“…deep breath every 2 hours.”
“…deep breath as needed.
Your Portfolio Chart
Now you will document in a note in your portfolio chart to become more familiar with how a documentation note works.
Select File > Select New Patient. Search for and select your portfolio chart (Lastname Firstname,Portfolio). Click on the Notes tab and click on New Note. At ‘Progress Note Title,’ begin typing in Scavenger (for Scavenger Hunt Activity Documentation) in the Progress Note Title field. The note should pull to the top. If not, scroll through the results and choose the note title called Scavenger Hunt Activity Documentation. Click on it and highlight the note. Leave the date, time and author of the note as it appears.

You will select your instructor as the expected co-signer. Click OK. Follow the instructions in the note and complete the documentation. When you are finished with the note, click OK. Place your mouse in the body of the note and right-click; select Sign Note Now. (Or you may click on the Action menu and select Sign Note Now.) You will need to sign the note using your Username.
Submit your work
Document your answers directly on this document as you complete the activity. When you are finished, save this document and upload it to your Learning Management System (LMS). If you have any questions about submitting your work to your LMS, please contact your instructor.
| 10 | Neehr Perfect Level I Scavenger Hunt: EHR Orientation v8 Archetype Innovations, LLC ©2017 |



